- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (192) +-
- Baby & Mom (1322) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3044) +-
- Beauty > Skin Care > whitening (307)
- Chemotherapy & Immune Response (883) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (289)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (192)
- HEMATOLOGY (39)
-
Medical Supplies (503)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (10)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (0)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2691)
+-
- Allergy & Sinus (95)
- Children's Health Care (54)
- Cough, Cold & Flu (277)
- Digestive Health & Nausea (233)
- Ear, Nose & Throat Care (179)
- Eye Care (124)
- Feminine Care (325)
- Foot Care (9)
- Orthopaedic Appliances (1)
- Pain Relief & Management (241)
- Pill Organizer (2)
- Skin Treatments (839)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3275)
+-
- Bath & Body (271)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (175)
- Eye Care (131)
- Feminine Care (374)
- Foot Care (17)
- Hair Care (472)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (22)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (65)
- Shaving & Grooming (65)
- Sun Care (80)
-
Prescription Drugs (2914)
+-
- Analgesics (181)
- Cardiovascular System (374)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (176)
- Gastrointestinal Tract (244)
- Gastrointestinal Tract > Hepatology > Liver treatment (62)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (46)
- NEUROLOGY (225)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (100)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (301) +-
- Vitamins & Minerals Supplements (1212) +-
Ex Tax: 297EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.
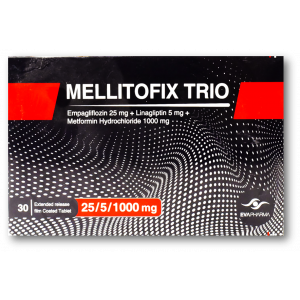
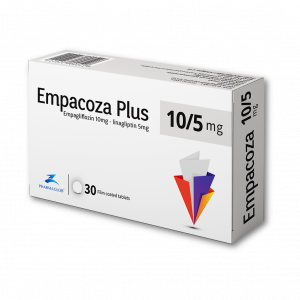
*Dosage Modifications
Hepatic impairment: No dosage adjustment required
Surgery:
- Withhold for at least 3 days, if possible, before major surgery or procedures associated with prolonged fasting
- Resume once patient is clinically stable and has resumed oral intake
Renal Impairment:
Type 2 diabetes mellitus
- eGFR 30-90 mL/min/1.73 m2: No dosage adjustment required
- eGFR <30 mL/min/1.73 m2 without cardiovascular (CV) risk factors: Not recommended
- Glucose lowering benefit of 25 mg/day decreased in patients with worsening renal function
- Risks of renal impairment, volume depletion adverse reactions and urinary tract infection-related adverse reactions increased with worsening renal function
T2DM and CV disease, HF, or CKD
- T2DM with CV disease GFR ≥30 mL/min/1.73 m2: No dosage adjustment required
- HF or CKD with eGFR ≥20 mL/min/1.73 m2: No dosage adjustment required
- eGFR <20 mL/min/1.73 m2 or on dialysis: Not studied
*Dosing Considerations
Limitations of use
- Not indicated for treatment of type 1 diabetes or diabetic ketoacidosis
- Not recommended for use to improve glycemic control in adults with type 2 diabetes mellitus with an eGFR <30 mL/min/1.73 m2
Before initiating therapy
- Assess renal function beforehand and periodically thereafter
- Correct condition in patients with volume depletion
Drug Interaction
- Contraindicated (0)
- Serious - Use Alternative (0)
- Monitor Closely (42):
amiloride
bendroflumethiazide
bumetanide
chlorothiazide
chlorpropamide
chlorthalidone
dulaglutide
ethacrynic acid
furosemide
glimepiride
glipizide
glyburide
hydrochlorothiazide
indapamide
insulin aspart
insulin aspart protamine/insulin aspart
insulin degludec
insulin degludec/insulin aspart
insulin detemir
insulin glargine
insulin glulisine
insulin inhaled
insulin isophane human/insulin regular human
insulin lispro
insulin lispro protamine/insulin lispro
insulin NPH
insulin regular human
letermovir
lithium
lonapegsomatropin
methyclothiazide
metolazone
nateglinide
repaglinide
somapacitan
somatrogon
somatropin
spironolactone
tolazamide
tolbutamide
torsemide
triamterene
- Minor (1): patiromer
Adverse Effects
- 1-10%
Urinary tract infection (7.6-9.3%)
Female genital mycotic infections (5.4-6.4%)
Upper respiratory tract infection (3.1-4%)
Increased urination (3.2-3.4%)
Dyslipidemia (2.9-3.9%)
Male genital mycotic infections (1.6-3.1%)
Arthralgia (2.3-2.4%)
Nausea (1.1-2.3%)
Polydipsia (1.5-1.7%)
- <1%
Adverse reactions related to volume depletion (eg, blood pressure [ambulatory] decreased, blood pressure systolic decreased, dehydration, hypotension, hypovolemia, orthostatic hypotension, and syncope)
Increased urination (eg, nocturia)
- Postmarketing reports
Ketoacidosis
Urosepsis and pyelonephritis
Necrotizing fasciitis of the perineum (Fournier’s gangrene)
Angioedema
Skin reactions
Acute kidney injury
Constipation
Diabetic ketoacidosis in patients with type 1 diabetes mellitus and other ketoacidosis
Warnings
Contraindications
Serious hypersensitivity to empagliflozin (eg, anaphylaxis, angioedema)
Cautions
Increases serum creatinine and decreases eGFR; risk increased in elderly or those with moderate renal impairment
Increased incidence of bone fractures reported; American Diabetes Association recommends avoiding sodium glucose cotransporter-2 inhibitors in patients with fracture risk factors
Genital mycotic infections may occur; patients with history of genital mycotic infections and uncircumcised males are more susceptible
Increases risk of urinary tract infections (UTIs), including life-threatening urosepsis and pyelonephritis that started as UTIs
Dose-related increases in LDL-C reported
No conclusive evidence of macrovascular risk reduction with antidiabetic agent
Serious hypersensitivity reactions (eg, angioedema) reported; if a hypersensitivity reaction occurs, discontinue treatment; treat promptly per standard of care, and monitor until signs and symptoms resolve
Volume depletion
- Intravascular volume depletion, which may manifest as symptomatic hypotension or acute changes in creatinine, occurred
- Acute kidney injury, some requiring hospitalization and dialysis, in patients with T2DM receiving SGLT2 inhibitors reported
- Patients with impaired renal function (eGFR <60 mL/min/1.73 m2), elderly patients, or patients on loop diuretics may be at increased risk for volume depletion or hypotension
- Before initiating therapy in patients with one or more of these characteristics, assess volume status and renal function; in patients with volume depletion, correct this condition before initiating treatment; monitor for signs and symptoms of volume depletion, and renal function after initiating therapy
Renal function
- Acute kidney injury reported
- Consider risk factors, including hypovolemia, heart failure, and chronic renal insufficiency or use of medications, including diuretics, ACE inhibitors, NSAIDs, or angiotensin receptor blockers
- Correct volume status before initiating if needed and monitor renal function periodically thereafter
Necrotizing fasciitis
- Necrotizing fasciitis of the perineum (Fournier gangrene) reported with SGLT2 inhibitors
- Signs and symptoms include pain or tenderness, erythema, or swelling in genital or perineal area, along with fever or malaise
- If suspected, discontinue SGLT2 inhibitor and start treatment immediately with broad-spectrum antibiotics and surgical debridement if necessary
Ketoacidosis
- Ketoacidosis, including fatal cases, reported in patients treated with SGLT2 inhibitors
- Not indicated for treatment of type 1 diabetes mellitus
- Before initiating therapy, consider factors in patient history that may predispose to ketoacidosis, including pancreatic insulin deficiency from any cause, caloric restriction, and alcohol abuse
- Consider temporarily discontinuing therapy for at least 3 days for patients who undergo scheduled surgery
- Consider monitoring for ketoacidosis and temporarily discontinuing therapy in other clinical situations known to predispose to ketoacidosis (eg, prolonged fasting due to acute illness or post-surgery); ensure risk factors for ketoacidosis are resolved prior to restarting therapy
- Restart once the patient’s oral intake is back to baseline and any other risk factors for ketoacidosis (blood acid buildup) are resolved
- Type 2 diabetes mellitus and pancreatic disorders (eg, history of pancreatitis or pancreatic surgery) are also risk factors for ketoacidosis. There have been postmarketing reports of fatal events of ketoacidosis in patients with type 2 diabetes mellitus using SGLT2 inhibitors.
- Precipitating conditions for diabetic ketoacidosis or other ketoacidosis include under-insulinization due to insulin dose reduction or missed insulin doses, acute febrile illness, reduced caloric intake, ketogenic diet, surgery, volume depletion, and alcohol abuse
- Ketoacidosis and glucosuria may persist longer than typically expected; urinary glucose excretion persists for 3 days after discontinuing therapy; however, there have been postmarketing reports of ketoacidosis and/or glucosuria lasting greater than 6 days and some up to 2 weeks after discontinuation of SGLT2 inhibitors
- Consider ketone monitoring in patients at risk for ketoacidosis if indicated by the clinical situation; assess for ketoacidosis regardless of presenting blood glucose levels in patients who present with signs and symptoms consistent with severe metabolic acidosis; if ketoacidosis is suspected, discontinue therapy, promptly evaluate, and treat ketoacidosis, if confirmed; monitor patients for resolution of ketoacidosis before restarting therapy
- Educate all patients on signs and symptoms of ketoacidosis and instruct patients to discontinue therapy and seek medical attention immediately if signs and symptoms occur
Drug interactions overview
- Insulin and insulin secretagogues:
- Modify dose/monitor
- Hypoglycemia risk increased with insulin and insulin secretagogues (eg, sulfonylureas); consider reducing dose of insulin or insulin secretagogue
- In adults, risk of hypoglycemia may be increased when empagliflozin is used in combination with insulin secretagogues (eg, sulfonylurea) or insulin
- In pediatric patients aged >10 years, the risk of hypoglycemia was higher with therapy regardless of insulin use
- Risk of hypoglycemia may be lowered by reducing dose of sulfonylurea (or other concomitantly administered insulin secretagogues) or insulin
- Inform patients using these concomitant medications and pediatric patients of risk of hypoglycemia and educate them on signs and symptoms of hypoglycemia
- Laboratory testing:
- Urine glucose tests is not recommended in patients taking SGLT2 inhibitors, as SGLT2 inhibitors, increase urinary glucose excretion and lead to positive urine glucose tests; use alternative methods to monitor glycemic control
- 1,5-AG assay is not recommended, as measurements of 1,5-AG are unreliable in assessing glycemic control in patients taking SGLT2 inhibitors; use alternative methods to monitor glycemic control
Pregnancy & Lactation
- Pregnancy
Based on animal data showing adverse renal effects, use not recommended during the second and third trimesters of pregnancy
Limited data available in pregnant women are insufficient to determine a drug-associated risk for major birth defects and miscarriage
There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy
Animal data
- In animal studies, adverse renal changes were observed in rats when empagliflozin was administered during period of renal development corresponding to the late second and third trimesters of human pregnancy
- Doses ~13-times the maximum clinical dose caused renal pelvic and tubule dilatations were reversible
- Not teratogenic in rats and rabbits up to 300 mg/kg/day, which approximates 48-times and 128-times, respectively, the maximum clinical dose of 25 mg when administered during organogenesis
Clinical considerations
Poorly controlled diabetes in pregnancy increases maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, stillbirth, and delivery complications; poorly controlled diabetes increases fetal risk for major birth defects, still birth, and macrosomia related morbidity
- Lactation
There is no information regarding presence in human milk, the effects on breastfed infant or on milk production
Empagliflozin is present in the milk of lactating rats
Because of potential for serious adverse reactions in a breastfed infant, advise women that it is not recommended while breastfeeding
*Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk.
C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done.
D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk.
X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist.
NA: Information not available.
Pharmacology
Mechanism of Action
Selective sodium-glucose transporter-2 (SGLT2) inhibitor
SGLT2 is expressed in the proximal renal tubules and is responsible for the majority of the reabsorption of filtered glucose from the tubular lumen; SGLT2 inhibitors reduce glucose reabsorption and lower the renal threshold for glucose, thereby increasing urinary glucose excretion
Also reduces sodium reabsorption and increases the delivery of sodium to the distal tubule; this may influence several physiological functions, such as lowering both pre-and afterload of the heart and downregulating sympathetic activity
Absorption
Peak plasma time: 1.5 hr
Peak plasma concentration: 259 nmol/L (10 mg/day); 687 nmol/L (25 mg/day)
AUC: 1870 nmol•hr/L (10 mg/day); 4740 nmol•hr/L (25 mg/day)
Distribution
Protein bound: 86.2%
Red blood cell partitioning: 36.8%
Vd: 73.8 L
Metabolism
Primary route of metabolism is glucuronidation by the uridine 5'-diphospho-glucuronosyltransferases UGT2B7, UGT1A3, UGT1A8, and UGT1A9
No major metabolites were detected and the most abundant metabolites were 3 glucuronide conjugates (2-O-, 3-O-, and 6-O-glucuronide)
Systemic exposure of each metabolite was <10%
Elimination
Half-life: 12.4 hr
Clearance: 10.6 L/hr
Excretion: 54.4% urine; 41.2% feces
Administration
Oral Administration
May take with or without food
Advise patient to have adequate fluid intake to decreased risk of hypotension
Missed dose
- Take missed dose as soon as possible
- Do not double next dose
Storage
Store at 25ºC (77ºF); excursions permitted to 15-30ºC (59-86ºF)
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: