- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (197) +-
- Baby & Mom (1346) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3129) +-
- Beauty > Skin Care > whitening (309)
- Chemotherapy & Immune Response (885) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (290)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (191)
- HEMATOLOGY (39)
-
Medical Supplies (506)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (11)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (1)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2727)
+-
- Allergy & Sinus (97)
- Children's Health Care (54)
- Cough, Cold & Flu (283)
- Digestive Health & Nausea (231)
- Ear, Nose & Throat Care (181)
- Eye Care (124)
- Feminine Care (323)
- Foot Care (12)
- Orthopaedic Appliances (1)
- Pain Relief & Management (244)
- Pill Organizer (2)
- Skin Treatments (863)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3363)
+-
- Bath & Body (273)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (177)
- Eye Care (131)
- Feminine Care (372)
- Foot Care (20)
- Hair Care (511)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (26)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (64)
- Shaving & Grooming (75)
- Sun Care (80)
-
Prescription Drugs (2935)
+-
- Analgesics (184)
- Cardiovascular System (377)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (177)
- Gastrointestinal Tract (243)
- Gastrointestinal Tract > Hepatology > Liver treatment (60)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (47)
- NEUROLOGY (228)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (115)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (304) +-
- Vitamins & Minerals Supplements (1230) +-
Ex Tax: 3,800EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

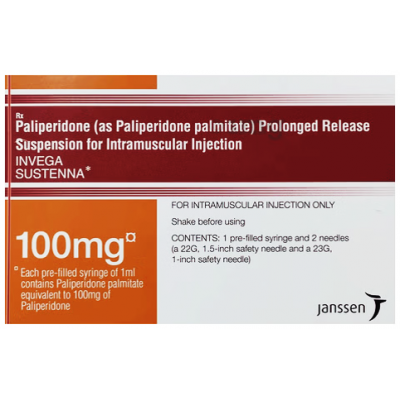
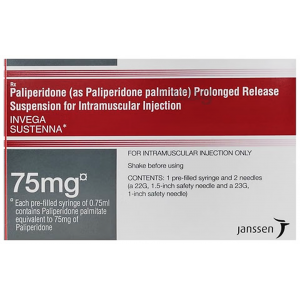
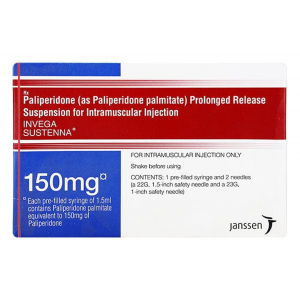
INVEGA SUSTENNA ® 100 MG / ML ( PALIPERIDONE PALMITATE ) 1 ML INTRAMASCULAR PRE-FILLED SYRINGE
INDICATION
INVEGA HAFYERA®, an every-six-month injection, is an atypical antipsychotic indicated for the treatment of schizophrenia in adults after they have been adequately treated with:
- A once-a-month paliperidone palmitate extended release injectable suspension (e.g., INVEGA SUSTENNA®) for at least four months or
- An every-three-month paliperidone palmitate extended release injectable suspension (e.g., INVEGA TRINZA®) for at least one three-month cycle.
INVEGA TRINZA® is an atypical antipsychotic indicated for the treatment of schizophrenia in patients after they have been adequately treated with INVEGA SUSTENNA® for at least four months.
INVEGA SUSTENNA® is an atypical antipsychotic indicated for the treatment of schizophrenia in adults.
IMPORTANT SAFETY INFORMATION
|
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS. See full prescribing information for complete Boxed Warning. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® are not approved for use in patients with dementia-related psychosis. |
Contraindications: INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® are contraindicated in patients with a known hypersensitivity to either paliperidone, risperidone, or to any excipients of their formulation.
Cerebrovascular Adverse Reactions: Cerebrovascular adverse reactions (e.g., stroke, transient ischemic attacks), including fatalities, were reported at a higher incidence in elderly patients with dementia-related psychosis taking risperidone, aripiprazole, and olanzapine compared to placebo. No studies have been conducted with oral paliperidone, INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® in elderly patients with dementia. These medications are not approved for the treatment of patients with dementia-related psychosis.
Neuroleptic Malignant Syndrome (NMS): NMS, a potentially fatal symptom complex, has been reported in association with antipsychotic drugs, including paliperidone.
Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status including delirium, and autonomic instability (irregular pulse of blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
If NMS is suspected, immediately discontinue INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® and provide symptomatic treatment and monitoring.
QT Prolongation: Paliperidone causes a modest increase in the corrected QT (QTc) interval. Avoid the use of drugs that also increase QTc interval and in patients with risk factors for prolonged QTc interval. Paliperidone should also be avoided in patients with congenital long QT syndrome and in patients with a history of cardiac arrhythmias. Certain circumstances may increase the risk of the occurrence of torsades de pointes and/or sudden death in association with the use of drugs that prolong the QTc interval.
Tardive Dyskinesia (TD): TD, a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements, may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to predict which patients will develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing TD and the likelihood that it will become irreversible appear to increase with the duration of treatment and the cumulative dose. The syndrome can develop after relatively brief treatment periods, even at low doses. It may also occur after discontinuation. TD may remit, partially or completely, if antipsychotic treatment is discontinued. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome, possibly masking the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
If signs and symptoms of TD appear in a patient on INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA®, drug discontinuation should be considered. However, some patients may require treatment with INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® despite the presence of the syndrome. In patients who do require chronic treatment, use the lowest dose and the shortest duration of treatment producing a satisfactory clinical response. Periodically reassess the need for continued treatment.
Metabolic Changes: Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain. While all of the drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia and Diabetes Mellitus: Hyperglycemia and diabetes mellitus, in some cases extreme and associated with ketoacidosis, hyperosmolar coma or death, have been reported in patients treated with all atypical antipsychotics (APS). Patients starting treatment with APS who have or are at risk for diabetes mellitus should undergo fasting blood glucose testing at the beginning of and during treatment. Patients who develop symptoms of hyperglycemia during treatment should also undergo fasting blood glucose testing. All patients treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia. Some patients require continuation of antidiabetic treatment despite discontinuation of the suspect drug.
Dyslipidemia: Undesirable alterations have been observed in patients treated with atypical antipsychotics.
Weight Gain: Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Orthostatic Hypotension and Syncope: INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® may induce orthostatic hypotension in some patients due to its alpha-adrenergic blocking activity. INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® should be used with caution in patients with known cardiovascular disease, cerebrovascular disease or conditions that would predispose patients to hypotension (e.g., dehydration, hypovolemia, treatment with antihypertensive medications). Monitoring should be considered in patients for whom this may be of concern.
Falls: Somnolence, postural hypotension, motor and sensory instability have been reported with the use of antipsychotics, including INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA®, which may lead to falls and, consequently, fractures or other fall-related injuries. For patients, particularly the elderly, with diseases, conditions, or medications that could exacerbate these effects, assess the risk of falls when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
Leukopenia, Neutropenia and Agranulocytosis have been reported with antipsychotics, including INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA®. In patients with a history of clinically significant low white blood cell count (WBC)/absolute neutrophil count (ANC) or drug-induced leukopenia/neutropenia, perform a complete blood count frequently during the first few months of therapy. Consider discontinuing INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® at the first sign of a clinically significant decline in WBC in the absence of other causative factors. Monitor patients with clinically significant neutropenia for fever or other symptoms or signs of infection and treat promptly if such symptoms or signs occur. Discontinue INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® in patients with severe neutropenia (absolute neutrophil count <1000/mm3) and follow their WBC until recovery.
Hyperprolactinemia: As with other drugs that antagonize dopamine D2 receptors, INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® elevate prolactin levels, and the elevation persists during chronic administration. Paliperidone has a prolactin-elevating effect similar to risperidone, which is associated with higher levels of prolactin elevation than other antipsychotic agents.
Potential for Cognitive and Motor Impairment: Somnolence, sedation, and dizziness were reported as adverse reactions in subjects treated with INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA®. INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® have the potential to impair judgment, thinking, or motor skills. Patients should be cautioned about performing activities that require mental alertness such as operating hazardous machinery, including motor vehicles, until they are reasonably certain that INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® do not adversely affect them.
Seizures: INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® should be used cautiously in patients with a history of seizures or with conditions that potentially lower seizure threshold. Conditions that lower seizure threshold may be more prevalent in patients 65 years or older.
Administration: For intramuscular injection only by a healthcare professional using only the needles provided in the INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® kits. Care should be taken to avoid inadvertent injection into a blood vessel.
Drug Interactions: Strong CYP3A4/P-glycoprotein (P-gp) inducers: Avoid using a strong inducer of CYP3A4 and/or P-gp (e.g., carbamazepine, rifampin, St John’s Wort) during a dosing interval for INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA®. If administering a strong inducer is necessary, consider managing the patient using paliperidone extended-release tablets.
Pregnancy/Nursing: INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® may cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. Advise patients to notify their healthcare professional if they become pregnant or intend to become pregnant during treatment with INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA®. Patients should be advised that there is a pregnancy registry that monitors outcomes in women exposed to INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® during pregnancy. INVEGA HAFYERA®, INVEGA TRINZA® and INVEGA SUSTENNA® can pass into human breast milk. The benefits of breastfeeding should be considered along with the mother’s clinical need for INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® and any potential adverse effect on the breastfed infant from INVEGA HAFYERA®, INVEGA TRINZA® or INVEGA SUSTENNA® or the mother’s underlying condition.
Commonly Observed Adverse Reactions for INVEGA HAFYERA®: The most common adverse reactions (incidence at least 5% in the double-blind phase) in the INVEGA HAFYERA® clinical trial were upper respiratory tract infection, injection site reaction, weight increased, headache and parkinsonism.
Commonly Observed Adverse Reactions for INVEGA TRINZA®: The most common adverse reactions (incidence ≥ 5% and occurring at least twice as often as placebo) were injection site reaction, weight increased, headache, upper respiratory tract infection, akathisia and parkinsonism.
Commonly Observed Adverse Reactions for INVEGA SUSTENNA®: The most common adverse reactions in clinical trials in patients with schizophrenia (incidence ≥ 5% and occurring at least twice as often as placebo) were injection site reactions, somnolence/sedation, dizziness, akathisia and extrapyramidal disorder.
Please read the full Prescribing Information, including Boxed WARNING, for INVEGA HAFYERA®, read the full Prescribing Information, including Boxed WARNING, for INVEGA TRINZA® and read the full Prescribing Information, including Boxed WARNING, for INVEGA SUSTENNA®.
--Brand Name--
US Brand Name:
- Erzofri
- Invega Hafyera
- Invega Sustenna
- Invega Trinza
--Description--
Paliperidone injection is used to treat the symptoms of psychotic (mental) disorders, including schizophrenia. Invega Trinza® and Invega Hafyera® are used if patients have been treated with Invega Sustenna® for at least 4 months. Invega Hafyera® is also used if patients have been treated with Invega Trinza® for at least 3 months. Invega Sustenna® may also be used alone or in combination with other medicines to treat schizoaffective disorder. This medicine should not be used to treat behavioral problems in older adults who have dementia.
This medicine is to be given only by or under the direct supervision of your doctor.
This product is available in the following dosage forms: Suspension, Extended Release
--Before Using--
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of paliperidone injection in the pediatric population. Use of Invega Trinza® or Invega Hafyera® is not recommended. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of paliperidone injection in the elderly. However, elderly patients are more likely to have age-related kidney problems, which may require caution and an adjustment in the dose for patients receiving paliperidone injection.
Breastfeeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Bepridil
- Bromopride
- Cisapride
- Dronedarone
- Levoketoconazole
- Mesoridazine
- Metoclopramide
- Pimozide
- Piperaquine
- Saquinavir
- Sparfloxacin
- Terfenadine
- Thioridazine
- Ziprasidone
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acecainide
- Acepromazine
- Adagrasib
- Ajmaline
- Alfentanil
- Alfuzosin
- Alprazolam
- Amiodarone
- Amisulpride
- Amitriptyline
- Amobarbital
- Amoxapine
- Anagrelide
- Anileridine
- Apalutamide
- Apomorphine
- Aripiprazole
- Aripiprazole Lauroxil
- Arsenic Trioxide
- Artemether
- Asenapine
- Astemizole
- Atazanavir
- Azithromycin
- Baclofen
- Bedaquiline
- Benperidol
- Benzhydrocodone
- Bretylium
- Bromazepam
- Bromocriptine Mesylate
- Buprenorphine
- Buserelin
- Buspirone
- Butabarbital
- Butorphanol
- Cabergoline
- Calcium Oxybate
- Cannabidiol
- Cannabis
- Carbamazepine
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chloroquine
- Chlorpromazine
- Chlorzoxazone
- Ciprofloxacin
- Citalopram
- Clarithromycin
- Clobazam
- Clofazimine
- Clomipramine
- Clonazepam
- Clorazepate
- Clothiapine
- Clozapine
- Codeine
- Crizotinib
- Cyclobenzaprine
- Dabrafenib
- Daridorexant
- Dasatinib
- Degarelix
- Delamanid
- Desflurane
- Desipramine
- Deslorelin
- Deutetrabenazine
- Dexmedetomidine
- Diacetylmorphine
- Diazepam
- Dichloralphenazone
- Difenoxin
- Dihydrocodeine
- Diphenhydramine
- Diphenoxylate
- Disopyramide
- Dofetilide
- Dolasetron
- Domperidone
- Donepezil
- Doxepin
- Doxylamine
- Droperidol
- Ebastine
- Efavirenz
- Encorafenib
- Enflurane
- Entrectinib
- Enzalutamide
- Eribulin
- Erythromycin
- Escitalopram
- Esketamine
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Etrasimod
- Famotidine
- Felbamate
- Fenoldopam Mesylate
- Fentanyl
- Fexinidazole
- Fingolimod
- Flecainide
- Flibanserin
- Fluconazole
- Flunitrazepam
- Fluoxetine
- Fluphenazine
- Flurazepam
- Fluspirilene
- Formoterol
- Foscarnet
- Fosphenytoin
- Fospropofol
- Fostemsavir
- Gabapentin
- Gabapentin Enacarbil
- Galantamine
- Gatifloxacin
- Gemifloxacin
- Gepirone
- Gepotidacin
- Givinostat
- Glasdegib
- Gonadorelin
- Goserelin
- Granisetron
- Halazepam
- Halofantrine
- Haloperidol
- Halothane
- Hexobarbital
- Histrelin
- Hydrocodone
- Hydromorphone
- Hydroquinidine
- Hydroxychloroquine
- Hydroxyzine
- Ibutilide
- Iloperidone
- Imipramine
- Inotuzumab Ozogamicin
- Insulin Aspart, Recombinant
- Isoflurane
- Itraconazole
- Ivabradine
- Ivacaftor
- Ivosidenib
- Ketamine
- Ketazolam
- Ketobemidone
- Ketoconazole
- Lapatinib
- Lefamulin
- Lenvatinib
- Leuprolide
- Levocetirizine
- Levodopa
- Levofloxacin
- Levorphanol
- Lofexidine
- Lonafarnib
- Lopinavir
- Lorazepam
- Lorlatinib
- Loxapine
- Lumacaftor
- Lumefantrine
- Macimorelin
- Magnesium Oxybate
- Mavorixafor
- Meclizine
- Mefloquine
- Melperone
- Meperidine
- Mephobarbital
- Meprobamate
- Meptazinol
- Metaxalone
- Methadone
- Methdilazine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Methylene Blue
- Metronidazole
- Midazolam
- Mifepristone
- Mirtazapine
- Mitotane
- Mizolastine
- Mobocertinib
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Moxifloxacin
- Nafarelin
- Nalbuphine
- Nelfinavir
- Nicomorphine
- Nilotinib
- Nitrazepam
- Nitrous Oxide
- Norfloxacin
- Nortriptyline
- Octreotide
- Ofloxacin
- Olanzapine
- Ondansetron
- Opium
- Opium Alkaloids
- Orphenadrine
- Osilodrostat
- Osimertinib
- Oxaliplatin
- Oxazepam
- Oxycodone
- Oxymorphone
- Ozanimod
- Pacritinib
- Panobinostat
- Papaveretum
- Papaverine
- Paregoric
- Paroxetine
- Pasireotide
- Pazopanib
- Pentamidine
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenobarbital
- Phenytoin
- Pimavanserin
- Pipamperone
- Piperacetazine
- Pipotiazine
- Piritramide
- Pitolisant
- Ponesimod
- Posaconazole
- Potassium Oxybate
- Prajmaline
- Pramipexole Dihydrochloride
- Prazepam
- Probucol
- Procainamide
- Prochlorperazine
- Promazine
- Promethazine
- Propafenone
- Propofol
- Protriptyline
- Quazepam
- Quetiapine
- Quinidine
- Quinine
- Quizartinib
- Ramelteon
- Ranolazine
- Relugolix
- Remifentanil
- Remimazolam
- Remoxipride
- Revumenib
- Ribociclib
- Rifabutin
- Rifampin
- Rifapentine
- Rilpivirine
- Risperidone
- Ritonavir
- Ropinirole Hydrochloride
- Rotigotine
- Secobarbital
- Selpercatinib
- Sertindole
- Sertraline
- Sevoflurane
- Simeprevir
- Siponimod
- Sodium Oxybate
- Sodium Phosphate
- Sodium Phosphate, Dibasic
- Sodium Phosphate, Monobasic
- Solifenacin
- Sorafenib
- Sotalol
- Sparteine
- St John's Wort
- Sufentanil
- Sulpiride
- Sultopride
- Sunitinib
- Suvorexant
- Tacrolimus
- Taletrectinib
- Tamoxifen
- Tapentadol
- Tedisamil
- Telaprevir
- Telavancin
- Telithromycin
- Temazepam
- Tetrabenazine
- Thiethylperazine
- Thiopental
- Thiopropazate
- Tilidine
- Tipranavir
- Tizanidine
- Tolonium Chloride
- Tolterodine
- Topiramate
- Toremifene
- Tramadol
- Trazodone
- Triazolam
- Triclabendazole
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Trimipramine
- Triptorelin
- Vandetanib
- Vardenafil
- Vemurafenib
- Venlafaxine
- Vilanterol
- Vinflunine
- Voclosporin
- Voriconazole
- Vorinostat
- Zaleplon
- Zolpidem
- Zopiclone
- Zotepine
- Zuclopenthixol
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Blood or bone marrow problems (eg, leukopenia, neutropenia) or
- Breast cancer, prolactin-dependent or
- Diabetes or
- Dyslipidemia (high cholesterol or fats in the blood) or
- Hyperglycemia (high blood sugar) or
- Hyperprolactinemia (high prolactin in the blood) or
- Neuroleptic malignant syndrome (NMS), history of or
- Priapism (painful or prolonged erection of the penis) or
- Seizures, history of—Use with caution. May make these conditions worse.
- Bradycardia (slow heartbeat) or
- Heart rhythm problems (eg, arrhythmia, QT prolongation), or history of or
- Hypokalemia (low potassium in the blood) or
- Hypomagnesemia (low magnesium in the blood)—Use with caution. May increase risk for more serious side effects.
- Dehydration or
- Dementia or
- Heart attack, recent or history of or
- Heart failure or
- Heart or blood vessel disease or
- Hypotension (low blood pressure) or
- Hypovolemia (low amount of blood) or
- Ischemic heart disease, history of or
- Stroke, history of or
- Trouble with swallowing—Use with caution. May cause side effects to become worse.
- Kidney disease, mild—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Kidney disease, moderate or severe—Use is not recommended in patients with this condition.
- Lewy body dementia or
- Parkinson's disease—Use with caution. Patients with these conditions may have increased sensitivity to the effects of this medicine.
--Proper Use--
A nurse or other trained health professional will give you this medicine in a medical facility. It is given as a shot into one of your muscles, usually in the arms or buttocks.
This medicine should come with a patient information leaflet. Read and follow these instructions carefully. Ask your doctor if you have any questions.
When you receive the first dose of Invega Sustenna®, you will need to get a second dose 1 week later. After that, you will only need to get a dose once a month. You will receive Invega Trinza® once every 3 months and Invega Hafyera® once every 6 months.
--Precautions--
It is very important that your doctor check your progress at regular visits to make sure that this medicine is working properly. Blood tests may be needed to check for any unwanted effects.
This medicine may raise your risk of having a stroke. This is more likely in people who already have heart or blood vessel disease. Check with your doctor right away if you are having confusion, difficulty in speaking, slow speech, inability to speak or move the arms, legs, or facial muscles, double vision, or headache.
Check with your doctor right away if you have difficulty with breathing, a fast heartbeat, a high fever, high or low blood pressure, increased sweating, loss of bladder control, seizures, severe muscle stiffness, unusually pale skin, or tiredness. These could be symptoms of a serious condition called neuroleptic malignant syndrome (NMS).
This medicine may cause tardive dyskinesia (a movement disorder). Check with your doctor right away if you have lip smacking or puckering, puffing of the cheeks, rapid or worm-like movements of the tongue, uncontrolled chewing movements, or uncontrolled movements of the arms and legs.
This medicine can cause changes in heart rhythm, including QT prolongation. It may change the way your heart beats and cause fainting or serious side effects in some patients. Call your doctor right away if you have dizziness, feeling faint, or a fast, pounding, or irregular heartbeat.
This medicine may increase the amount of sugar in your blood. Check with your doctor right away if you have blurred vision, dry mouth, flushed, dry skin, increased hunger, increased thirst or urination, nausea, sweating, trouble breathing, unexplained weight loss, unusual tiredness or weakness, or vomiting. If you have diabetes, you may notice a change in the results of your urine or blood sugar tests. If you have any questions, check with your doctor.
This medicine may increase the amount of cholesterol and fats in your blood. If this condition occurs, your doctor may give you some medicines that can lower the amount of cholesterol and fats in the blood.
This medicine may increase prolactin blood levels if used for a long time. Check with your doctor if you have breast swelling or soreness, unusual breast milk production, absent, missed, or irregular menstrual periods, stopping of menstrual bleeding, loss in sexual ability, desire, drive, or performance, decreased interest in sexual intercourse, or an inability to have or keep an erection.
Dizziness, lightheadedness, or fainting may occur, especially when you suddenly get up from a lying or sitting position. Getting up slowly may help. If this problem continues or gets worse, check with your doctor.
Paliperidone injection can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. If you can, avoid people with infections. Check with your doctor right away if you think you are getting an infection, or if you have a fever or chills, cough or hoarseness, lower back or side pain, or painful or difficult urination.
This medicine may cause drowsiness, trouble with thinking, or trouble with controlling body movements, which may lead to falls, fractures, or other injuries. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
This medicine may cause difficulty swallowing that can cause food or liquid to get into your lungs and a prolonged or painful erection, which can last for more than 4 hours. Talk to your doctor if you have any concerns about this.
This medicine may make it more difficult for your body to cool itself down. Use care not to become overheated during exercise or hot weather since overheating may result in heat stroke. Also, use extra care not to become too cold while you are receiving risperidone injection. If you become too cold, you may feel drowsy, confused, or clumsy.
This medicine may increase your weight. Your doctor may need to check your weight on a regular basis while you are receiving this medicine. Talk to your doctor about ways to prevent weight gain.
Check with your doctor before using this medicine with alcohol or other medicines that affect the central nervous system (CNS). The use of alcohol or other medicines that affect the CNS with risperidone may worsen the side effects of this medicine, including dizziness, poor concentration, drowsiness, unusual dreams, and trouble with sleeping. Some examples of medicines that affect the CNS are antihistamines or medicine for allergies or colds, sedatives, tranquilizers, or sleeping medicines, medicine for depression, medicine for anxiety, prescription pain medicine or narcotics, medicine for attention deficit and hyperactivity disorder, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics.
If you plan to have children, talk with your doctor before using this medicine. Some women using this medicine have become infertile (unable to have children).
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
--Side Effects--
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor or nurse immediately if any of the following side effects occur:
More common
- Anxiety
- bladder pain
- bloody or cloudy urine
- body aches or pain
- chills
- cough
- deep or fast breathing with dizziness
- difficult, burning, or painful urination
- difficulty with breathing
- difficulty with swallowing
- dry mouth
- ear congestion
- fever
- frequent urge to urinate
- headache
- inability to sit still
- irregular heartbeat
- irritability
- loss of balance control
- loss of voice
- lower back or side pain
- mask-like face
- need to keep moving
- nervousness
- numbness of the feet, hands, and around the mouth
- restlessness
- runny or stuffy nose
- shaking
- shuffling walk
- slowed movements
- slurred speech
- sneezing
- sore throat
- stiffness of the arms and legs
- tic-like (jerky) movements of the head, face, mouth, and neck
- trembling and shaking of the fingers and hands
- trouble with sleeping
- twitching, twisting, uncontrolled repetitive movements of the tongue, lips, face, arms, or legs
- unusual tiredness or weakness
Less common
- Blurred vision
- difficulty with speaking
- dizziness
- drooling
- inability to move the eyes
- increase in body movements
- increased blinking or spasms of the eyelid
- loss of balance control
- muscle trembling, jerking, or stiffness
- pounding in the ears
- slow or fast heartbeat
- sticking out of the tongue
- uncontrolled movements, especially of the face, neck, and back
- uncontrolled twisting movements of the neck, trunk, arms, or legs
- unusual facial expressions
Incidence not known
- Change in mental status
- chest tightness
- decrease in the amount and frequency of urination
- difficulty speaking
- hives, itching, skin rash
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- loss of bladder control
- pale color of the skin
- pinpoint red spots on the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- seizures
- severe constipation
- severe vomiting
- stomach pain
- swollen tongue
- yellow eyes or skin
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Bleeding, blistering, burning, coldness, discoloration of the skin, feeling of pressure, hives, infection, inflammation, itching, lumps, numbness, pain, rash, redness, scarring, soreness, stinging, swelling, tenderness, tingling, ulceration, or warmth at the injection site
Less common
- Back pain
- constipation
- diarrhea
- difficulty with moving
- dry mouth
- increased weight
- lack or loss of strength
- muscle pains, cramps, or stiffness
- nausea
- nightmares
- pain and swelling in the joints
- pain in the arms or legs
- tearing of the skin
- toothache
- upper abdominal or stomach pain
- vomiting
Incidence not known
- Sleepwalking
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: