- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (197) +-
- Baby & Mom (1346) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3129) +-
- Beauty > Skin Care > whitening (309)
- Chemotherapy & Immune Response (885) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (290)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (191)
- HEMATOLOGY (39)
-
Medical Supplies (506)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (11)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (1)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2727)
+-
- Allergy & Sinus (97)
- Children's Health Care (54)
- Cough, Cold & Flu (283)
- Digestive Health & Nausea (231)
- Ear, Nose & Throat Care (181)
- Eye Care (124)
- Feminine Care (323)
- Foot Care (12)
- Orthopaedic Appliances (1)
- Pain Relief & Management (244)
- Pill Organizer (2)
- Skin Treatments (863)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3363)
+-
- Bath & Body (273)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (177)
- Eye Care (131)
- Feminine Care (372)
- Foot Care (20)
- Hair Care (511)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (26)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (64)
- Shaving & Grooming (75)
- Sun Care (80)
-
Prescription Drugs (2935)
+-
- Analgesics (184)
- Cardiovascular System (377)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (177)
- Gastrointestinal Tract (243)
- Gastrointestinal Tract > Hepatology > Liver treatment (60)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (47)
- NEUROLOGY (228)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (115)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (304) +-
- Vitamins & Minerals Supplements (1232) +-
Ex Tax: 48,824EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

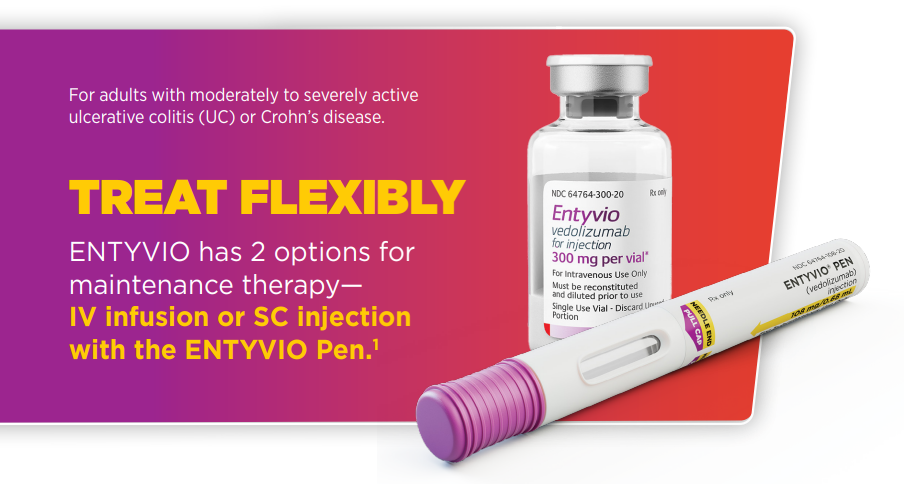
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
ENTYVIO is contraindicated in patients who have had a known serious or severe hypersensitivity reaction to ENTYVIO or any
of its excipients.
WARNINGS AND PRECAUTIONS
• Infusion-Related and Hypersensitivity Reactions: Infusion-related reactions and hypersensitivity reactions including
anaphylaxis, dyspnea, bronchospasm, urticaria, flushing, rash, and increased blood pressure and heart rate have been reported.
These reactions may occur with the first or subsequent infusions and may vary in their time of onset from during infusion or up
to several hours post-infusion. If anaphylaxis or other serious infusion-related or hypersensitivity reactions occur, discontinue
administration of ENTYVIO immediately and initiate appropriate treatment.
• Infections: Patients treated with ENTYVIO are at increased risk for developing infections. Serious infections have been reported
in patients treated with ENTYVIO, including anal abscess, sepsis (some fatal), tuberculosis, salmonella sepsis, Listeria meningitis,
giardiasis, and cytomegaloviral colitis. ENTYVIO is not recommended in patients with active, severe infections until the infections
are controlled. Consider withholding ENTYVIO in patients who develop a severe infection while on treatment with ENTYVIO.
Exercise caution in patients with a history of recurring severe infections. Consider screening for tuberculosis (TB) according to
the local practice.
• Progressive Multifocal Leukoencephalopathy (PML): PML, a rare and often fatal opportunistic infection of the central
nervous system (CNS), has been reported with systemic immunosuppressants, including another integrin receptor antagonist.
PML typically only occurs in patients who are immunocompromised. One case of PML in an ENTYVIO-treated patient with
multiple contributory factors has been reported. Although unlikely, a risk of PML cannot be ruled out. Monitor patients for
any new or worsening neurological signs or symptoms that may include progressive weakness on one side of the body or
clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality
changes. If PML is suspected, withhold dosing with ENTYVIO and refer to neurologist; if confirmed, discontinue ENTYVIO dosing
permanently.
• Liver Injury: There have been reports of elevations of transaminase and/or bilirubin in patients receiving ENTYVIO. ENTYVIO
should be discontinued in patients with jaundice or other evidence of significant liver injury.
• Live and Oral Vaccines: Prior to initiating treatment with ENTYVIO, all patients should be brought up to date with all
immunizations according to current immunization guidelines. Patients receiving ENTYVIO may receive non-live vaccines and
may receive live vaccines if the benefits outweigh the risks.
ADVERSE REACTIONS
The most common adverse reactions (incidence ≥3% and ≥1% higher than placebo) were: nasopharyngitis, headache, arthralgia,
nausea, pyrexia, upper respiratory tract infection, fatigue, cough, bronchitis, influenza, back pain, rash, pruritus, sinusitis,
oropharyngeal pain, pain in extremities, and injection site reactions with subcutaneous administration.
DRUG INTERACTIONS
Because of the potential for increased risk of PML and other infections, avoid the concomitant use of ENTYVIO with natalizumab
products and with TNF blockers. Upon initiation or discontinuation of ENTYVIO in patients treated with CYP450 substrates,
monitor drug concentrations or other therapeutic parameters, and adjust the dosage of the CYP substrate as needed.
INDICATIONS
Adult Ulcerative Colitis (UC):
ENTYVIO is indicated in adults for the treatment of moderately to severely active UC.
Adult Crohn’s Disease (CD):
ENTYVIO is indicated in adults for the treatment of moderately to severely active CD.
DOSAGE FORMS & STRENGTHS:
• ENTYVIO Intravenous (IV) Infusion: 300 mg vedolizumab
• ENTYVIO Subcutaneous (SC) Injection: 108 mg vedolizumab
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below:






