- Anti-hestaminic & Respiratory Drugs (17)
- Anti-inflammatory Drugs (170) +-
- Baby & Mom (1211) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (50)
- Beauty (2548) +-
- Beauty > Skin Care > whitening (259)
- Chemotherapy & Immune Response (476) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (4)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (155)
- CIRCULATORY DISTURBANCE AGENTS (19)
- Diet & Fitness Products (218) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (163)
- Drugs affecting CNS >Anti- epileptic (65)
-
Medical Supplies (470)
+-
- Chemicals & Disinfectants (17)
- Dental Supplies (27)
- Devices & Instruments (8)
- Diabetic Supplies (110)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- Kindney Unit Supplies (12)
- Lab Supplies (1)
- Miscellaneous (22)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (3)
- Sanitary (5)
- Sterilization Supplies (0)
- Surgical Sutures (3)
- Syringes (2)
-
Medicines & Health (2395)
+-
- Allergy & Sinus (91)
- Children's Health Care (52)
- Cough, Cold & Flu (282)
- Digestive Health & Nausea (201)
- Ear, Nose & Throat Care (159)
- Eye Care (114)
- Feminine Care (295)
- Foot Care (3)
- Orthopaedic Appliances (0)
- Pain Relief & Management (205)
- Pill Organizer (2)
- Skin Treatments (700)
- Sleep & Snoring Aids (0)
- Support & Braces (6)
- Medicines & health > Gout releif (41)
- Natural & Organic Products (78) +-
- OTC > Analgesics > Anti-inflammatory Drugs (43)
-
Personal Care (2835)
+-
- Bath & Body (214)
- Deodorant & Anti-perspirants (175)
- Ear, Nose & Throat Care (152)
- Eye Care (120)
- Feminine Care (332)
- Foot Care (11)
- Hair Care (374)
- Home Tests & Monitorings (16)
- Incontinence (7)
- Lip Care (19)
- Massage & Relaxation (18)
- Natural & Organic Personal Care (7)
- Oral Care (75)
- Pregnancy & Fertility (55)
- Shaving & Grooming (53)
- Sun Care (52)
- Prescribtion drugs > cardiovascular system > Hypertention drugs (323) +-
-
Prescription Drugs (2817)
+-
- Analgesics (172)
- Cardiovascular System (327)
- Drugs Affecting Musculoskeletal System (59)
- Drugs Used In Infections (49)
- Ear & Nose Drugs (2)
- Endocrine System (154)
- Gastrointestinal Tract (214)
- Gastrointestinal Tract (196)
- GYNECOLOGY (2)
- Miscellaneous (6)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (22)
- NEUROLOGY (190)
- Nutrients & Blood Electrolytes (2)
- prescription drugs > cardiovascular system >Anti-hypertensive drugs (72)
- Prescription Drugs > Gastrointestinal Tract > Hepatology > Liver treatment (55)
- Respiratory System (115)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (29)
- Vaccines (1)
- Sexual Wellness (196) +-
- strong anti-emetic & adjuvent used with anti-neoplastic (0)
- Vitamins & Minerals Supplements (1060) +-
Availability: In Stock
Ex Tax: 2,430EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

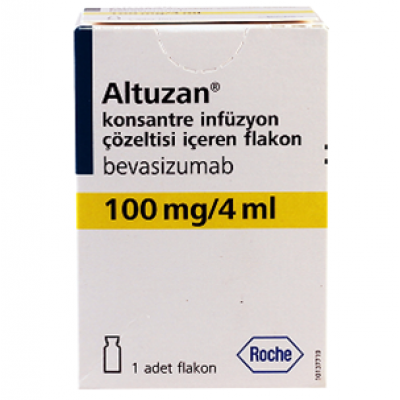
aLTUZAN 100 MG / 4 Ml ( humanised anti-VEGF monoclonal antibodY ) vIAL
WHAT IS ALTUZAN?
Altuzan injection is given with other medicines to treat patients with metastatic (a cancer that has spread) carcinoma of the colon or rectum. Altuzan is also used to treat a certain type of metastatic lung cancer called nonsquamous, non-small cell lung cancer, and a certain type of brain tumor called glioblastoma.
Altuzan is a substance that helps the body fight cancer. It prevents the growth of certain types of blood vessels to cancer cells. This helps to decrease the growth of cancer cells by starving the cells of nutrients that are needed to grow.
Altuzan injection is also used in combination with other medicines (eg, interferon alfa) to treat patients with cancer of the kidney that has spread to other areas of the body. It is also used in combination with other medicines (eg, paclitaxel and cisplatin, or paclitaxel and topotecan) to treat patients with cancer of the cervix that has spread to other areas of the body. Altuzan is also used in combination with other medicines (eg, paclitaxel, pegylated liposomal doxorubicin, or topotecan) to treat patients with platinum-resistant, recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Altuzan is to be given only by or under the immediate supervision of your doctor.
Once a medicine has been approved for marketing for a certain use, experience may show that it is also useful for other medical problems. Although these uses are not included in product labeling, Altuzan is used in certain patients with the following medical conditions:
- Diabetic macular edema (swelling of the back of the eye in diabetic patients).
- Glioblastoma multiforme, recurrent, after therapy with temozolomide (a type of brain cancer that is getting worse or not responding to therapy).
- Metastatic colorectal cancer, first-line therapy, in combination with capecitabine and oxaliplatin (cancer of the colon or rectum that has spread to other areas of the body).
ALTUZAN INDICATIONS
 An indication is a term used for the list of condition or symptom or illness for which the medicine is prescribed or used by the patient. For example, acetaminophen or paracetamol is used for fever by the patient, or the doctor prescribes it for a headache or body pains. Now fever, headache and body pains are the indications of paracetamol. A patient should be aware of the indications of medications used for common conditions because they can be taken over the counter in the pharmacy meaning without prescription by the Physician.
An indication is a term used for the list of condition or symptom or illness for which the medicine is prescribed or used by the patient. For example, acetaminophen or paracetamol is used for fever by the patient, or the doctor prescribes it for a headache or body pains. Now fever, headache and body pains are the indications of paracetamol. A patient should be aware of the indications of medications used for common conditions because they can be taken over the counter in the pharmacy meaning without prescription by the Physician.Metastatic Colorectal Cancer (mCRC)
Altuzan is indicated for the first- or second-line treatment of patients with metastatic carcinoma of the colon or rectum in combination with intravenous 5-fluorouracil–based chemotherapy.
Altuzan, in combination with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy, is indicated for the second-line treatment of patients with metastatic colorectal cancer who have progressed on a first-line Altuzan-containing regimen.
Limitation of Use: Altuzan is not indicated for adjuvant treatment of colon cancer.
Non-Squamous Non–Small Cell Lung Cancer (NSCLC)
Altuzan is indicated for the first-line treatment of unresectable, locally advanced, recurrent or metastatic non–squamous non–small cell lung cancer in combination with carboplatin and paclitaxel.
Glioblastoma
Altuzan is indicated for the treatment of glioblastoma with progressive disease in adult patients following prior therapy as a single agent.
The effectiveness of Altuzan in glioblastoma is based on an improvement in objective response rate. There are no data demonstrating an improvement in disease-related symptoms or increased survival with Altuzan.
Metastatic Renal Cell Carcinoma (mRCC)
Altuzan is indicated for the treatment of metastatic renal cell carcinoma in combination with interferon alfa.
Persistent, Recurrent, or Metastatic Carcinoma of the Cervix
Altuzan in combination with paclitaxel and cisplatin or paclitaxel and topotecan is indicated for the treatment of persistent, recurrent, or metastatic carcinoma of the cervix.
Platinum-Resistant Recurrent Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
Altuzan in combination with paclitaxel, pegylated liposomal doxorubicin or topotecan is indicated for the treatment of patients with platinum-resistant recurrent epithelial ovarian, fallopian tube or primary peritoneal cancer who received no more than 2 prior chemotherapy regimens.
HOW SHOULD I USE ALTUZAN?
Use Altuzan solution as directed by your doctor. Check the label on the medicine for exact dosing instructions.
- Altuzan solution is given as an injection at your doctor's office, hospital, or clinic. Contact your health care provider if you have any questions.
- If you miss a dose of Altuzan solution, contact your doctor immediately to establish a new dosing schedule.
Ask your health care provider any questions you may have about how to use Altuzan solution.
ALTUZAN DESCRIPTION:
Active Ingredient: Altuzan (humanised anti-VEGF monoclonal antibody).
Altuzan is supplied in 100 mg and 400 mg preservative-free, single-use vials containing 4 mL or 16 mL of Altuzan (25 mg/mL).
Each Altuzan 100 mg vial contains 100 mg of Altuzan.
Altuzan is not formulated for intravitreal use.
Excipients/Inactive Ingredients: α, α-trehalose dihydrate, sodium dihydrogen phosphate monohydrate, anhydrous disodium phosphate, polysorbate 20 and sterile water for injections.
ALTUZAN DOSAGE
General: Substitution by any other biological medicinal product requires the consent of the prescribing physician.
Altuzan should be prepared by a healthcare professional using aseptic technique.
The initial Altuzan dose should be delivered over 90 min as an IV infusion. If the 1st infusion is well-tolerated, the 2nd infusion may be administered over 60 min. If the 60-min infusion is well-tolerated, all subsequent infusions may be administered over 30 min.
Dose reduction of Altuzan for adverse events is not recommended. If indicated, Altuzan should either be permanently discontinued or temporarily suspended (Precautions).
Altuzan is not formulated for intravitreal use.
Metastatic Colorectal Cancer (mCRC): The recommended dose of Altuzan, administered as an IV infusion, is as follows: First-line Treatment: 5 mg/kg of body weight given once every 2 weeks or 7.5 mg/kg of body weight given once every 3 weeks. Second-line Treatment: 10 mg/kg of body weight given every 2 weeks or 15 mg/kg of body weight given once every 3 weeks.
It is recommended that Altuzan treatment be continued until progression of the underlying disease.
Locally Recurrent or Metastatic Breast Cancer (mBC): The recommended dose of Altuzan is 10 mg/kg of body weight given once every 2 weeks or 15 mg/kg of body weight given once every 3 weeks as an IV infusion. It is recommended that Altuzan treatment be continued until progression of the underlying disease.
Advanced, Metastatic or Recurrent Non-Small Cell Lung Cancer (NSCLC): Altuzan is administered in addition to platinum-based chemotherapy for up to 6 cycles of treatment followed by Altuzan as a single agent until disease progression.
The recommended dose of Altuzan when used in addition to cisplatin-based chemotherapy is 7.5 mg/kg of body weight given once every 3 weeks as an IV infusion.
The recommended dose of Altuzan when used in addition to carboplatin-based chemotherapy is 15 mg/kg of body weight given once every 3 weeks as an IV infusion.
Advanced and/or Metastatic Renal Cell Cancer (mRCC): The recommended dose of Altuzan is 10 mg/kg of body weight given once every 2 weeks as an IV infusion.
It is recommended that Altuzan treatment be continued until progression of the underlying disease.
Malignant Glioma (WHO Grade IV)-Glioblastoma: The recommended dose of Altuzan is 10 mg/kg of body weight given once every 2 weeks or 15 mg/kg of body weight given once every 3 weeks as an IV infusion.
It is recommended that Altuzan treatment be continued until progression of the underlying disease.
Epithelial Ovarian, Fallopian Tube and Primary Peritoneal Cancer: Altuzan is administered in addition to carboplatin and paclitaxel for up to 6 cycles of treatment followed by continued use of Altuzan as single agent for 15 months or until disease progression, whichever occurs earlier.
The recommended dose of Altuzan is 15 mg/kg of body weight given once every 3 weeks as an IV infusion.
Special Dosage Instructions: Children and Adolescents: The safety and efficacy of Altuzan in children and adolescents have not been studied.
ALTUZAN INTERACTIONS:
Effect of Antineoplastic Agents on Altuzan Pharmacokinetics: No clinically relevant pharmacokinetic interaction of co-administered chemotherapy on Altuzan pharmacokinetics has been observed based on the results of a population pharmacokinetics analysis. There was neither statistical significance nor clinically relevant difference in clearance of Altuzan in patients receiving Altuzan monotherapy compared to patients receiving Altuzan in combination with interferon α-2a or other chemotherapies (IFL, 5-FU/LV, carboplatin/paclitaxel, capecitabine, doxorubicin or cisplatin/gemcitabine).
Effect of Altuzan on the Pharmacokinetics of other Antineoplastic Agents: Results from a drug-drug interaction study, AVF3135g demonstrated no significant effect of Altuzan on the pharmacokinetics of irinotecan and its active metabolite SN38.
Results from NP18587 demonstrated no significant effect of Altuzan on the pharmacokinetics of capecitabine and its metabolites, and on the pharmacokinetics of oxaliplatin, as determined by measurement of free and total platinum.
Results from BO17705 demonstrated no significant effect of Altuzan on the pharmacokinetics of interferon α-2a.
Results from BO17704 demonstrated no significant effect of Altuzan on the pharmacokinetics of cisplatin. Due to high inter-patient variability and limited sampling, the results from BO17704 do not allow firm conclusions on the impact of Altuzan on gemcitabine pharmacokinetics to be drawn.
Combination of Altuzan and Sunitinib Malate: In 2 clinical studies of metastatic renal cell carcinoma, microangiopathic hemolytic anemia (MAHA) was reported in 7 of 19 patients treated with Altuzan (10 mg/kg every 2 weeks) and sunitinib malate (50 mg daily) combination.
Microangiopathic hemolytic anemia is a hemolytic disorder which can present with red cell fragmentation, anemia and thrombocytopenia. In addition, hypertension (including hypertensive crisis), elevated creatinine and neurological symptoms were observed in some of these patients. All of these findings were reversible upon discontinuation of Altuzan and sunitinib malate.
Radiotherapy: The safety and efficacy of concomitant administration of chemotherapy (temozolomide), radiotherapy and Altuzan was evaluated in study BO21990, a phase III, randomised, double-blind, placebo-controlled study of 921 patients with newly diagnosed glioblastoma. No new adverse events associated with Altuzan were reported in this study.
The safety and efficacy of concomitant administration of radiotherapy and Altuzan has not been established in other indications.
Incompatibilities: No incompatibilities between Altuzan and polyvinyl chloride or polyolefin bags have been observed. A concentration dependent degradation profile of Altuzan was observed when diluted with dextrose solutions (5%).
ALTUZAN SIDE EFFECTS:
Clinical Trials: Clinical trials have been conducted in patients with various malignancies treated with Altuzan, predominantly in combination with chemotherapy. The safety profile from a clinical trial population of approximately 5,200 patients is presented as follows. For post-marketing experience, see Post-Marketing as follows. See Clinical/Efficacy studies for details of major studies, including study designs and major efficacy results.
The most serious adverse drug reactions were: Gastrointestinal Perforations; haemorrhage including pulmonary haemorrhage/haemoptysis, which is more common in NSCLC patients; arterial thromboembolism.
Analyses of the clinical safety data suggest that the occurrence of hypertension and proteinuria with Altuzan therapy are likely to be dose-dependent.
The most frequently observed adverse drug reactions across clinical trials in patients receiving Altuzan were hypertension, fatigue or asthenia, diarrhea and abdominal pain.
Table 16 lists adverse drug reactions associated with the use of Altuzan in combination with different chemotherapy regimens in multiple indications. These reactions had occurred either with at least a 2% difference compared to the control arm (NCI-CTC grade 3-5 reactions) or with at least a 10% difference compared to the control arm (NCI-CTC grade 1-5 reactions), in at least one of the major clinical trials. The adverse drug reactions listed in Table 16 fall into the following categories: Very common (≥10%) and common (≥1% to <10%). Adverse drug reactions are added to the appropriate category in Table 16 according to the highest incidence seen in any of the major clinical trials. Within each frequency grouping, adverse drug reactions are presented in order of decreasing seriousness. Some of the adverse reactions are reactions commonly seen with chemotherapy however, Altuzan may exacerbate these reactions when combined with chemotherapeutic agents. Examples includes palmar-plantar erythrodysaesthesia syndrome with pegylated liposomal doxorubicin or capecitabine, peripheral sensory neuropathy with paclitaxel or oxaliplatin, and nail disorders or alopecia with paclitaxel.
Further Information on Selected Serious Adverse Drug Reactions: The following adverse drug reactions, reported using common toxicity criteria (NCI-CTC) for assessment of toxicity, have been observed in patients treated with Altuzan.
Gastrointestinal Perforation and Fistulae : Altuzan has been associated with serious cases of gastrointestinal perforation. Gastrointestinal perforations have been reported in clinical trials with an incidence of less than 1% in patients with metastatic breast cancer or non-squamous non-small cell lung cancer, and up to 2% in patients with metastatic renal cell cancer, newly diagnosed glioblastoma, or ovarian cancer receiving front-line treatment, and up to 2.7% (including gastrointestinal fistula and abscess) in patients with metastatic colorectal cancer. Cases of GI perforations have also been observed in patients with relapsed glioblastoma.
From a clinical trial in patients with persistent, recurrent, or metastatic cervical cancer (study GOG-0240), gastrointestinal perforation (all grade) were reported in 3.2% of patients, all of whom had a history of prior pelvic radiation.
The occurrence of those events varied in type and severity, ranging from free air seen on the plain abdominal X-ray, which resolved without treatment, to intestinal perforation with abdominal abscess and fatal outcome. In some cases, underlying intra-abdominal inflammation was present, either from gastric ulcer disease, tumour necrosis, diverticulitis or chemotherapy-associated colitis. A causal association of intra-abdominal inflammatory process and gastrointestinal perforation to Altuzan has not been established.
Fatal outcome was reported in approximately a 3rd of serious cases of gastrointestinal perforations, which represents between 0.2-1% of all Altuzan-treated patients.
In Altuzan clinical trials, gastrointestinal fistulae (all grade) have been reported with an incidence of up to 2% in patients with metastatic colorectal cancer and ovarian cancer, but were also reported less commonly in patients with other types of cancer.
In a trial of patients with persistent, recurrent or metastatic cervical cancer, the incidence of GI-vaginal fistulae was 8.3% in Altuzan-treated patients and 0.9% in control patients, all of whom had a history of prior pelvic radiation. Patients who develop GI-vaginal fistulae may also have bowel obstructions and require surgical intervention as well as diverting ostomies.
Non-GI Fistulae : Altuzan use has been associated with serious cases of fistulae including events resulting in death.
From a clinical trial in patients with persistent, recurrent, or metastatic cervical cancer (GOG-240), 1.8% of Altuzan-treated patients and 1.4% of control patients were reported to have had non-gastrointestinal vaginal, vesical, or female genital tract fistulae.
Uncommon (≥0.1% to <1%) reports of fistulae that involve areas of the body other than the gastrointestinal tract (eg, bronchopleural, biliary fistulae) were observed across various indications. Fistulae have also been reported in post-marketing experience.
Events were reported at various time points during treatment ranging from one week to greater than 1 year from initiation of Altuzan, with most events occurring within the first 6 months of therapy.
Hemorrhage: In clinical trials across all indications, the overall incidence of NCI-CTC grade 3-5 bleeding events ranged from 0.4-6.9% in Altuzan-treated patients, compared to 0-4.5% of patients in the chemotherapy control group. The haemorrhagic events that have been observed in Altuzan clinical studies were predominantly tumour-associated haemorrhage and minor mucocutaneous hemorrhage (eg, epistaxis).
Tumour-Associated Haemorrhage: Major or massive pulmonary haemorrhage/haemoptysis has been observed primarily in studies in patients with NSCLC. Possible risk factors include squamous cell histology, treatment with anti-rheumatic/anti-inflammatory drugs, treatment with anticoagulants, prior radiotherapy, Altuzan therapy, previous medical history of atherosclerosis, central tumour location and cavitation of tumours prior to or during therapy. The only variables that showed statistically significant correlations with bleeding were Altuzan therapy and squamous cell histology. Patients with NSCLC of known squamous cell histology or mixed cell type with predominant squamous cell histology were excluded from subsequent studies, while patients with unknown tumour histology were included.
In patients with NSCLC excluding predominant squamous histology, all Grade events were seen with a frequency of up to 9% when treated with Altuzan plus chemotherapy compared with 5% in the patients treated with chemotherapy alone. Grade 3-5 events have been observed in up to 2.3% of patients treated with Altuzan plus chemotherapy as compared with <1% with chemotherapy alone. Major or massive pulmonary haemorrhage/haemoptysis can occur suddenly and up to two thirds of the serious pulmonary haemorrhages resulted in a fatal outcome.
Gastrointestinal haemorrhages, including rectal bleeding and melaena have been reported in colorectal patients, and have been assessed as tumour-associated haemorrhages.
Tumour-associated haemorrhages were also seen rarely in other tumour types and locations and included cases of CNS bleeding in patients with hepatoma with CNS metastases and in patients with glioblastoma.
The incidence of CNS bleeding in patients with untreated CNS metastases receiving Altuzan has not been prospectively evaluated in randomised clinical studies. In an exploratory retrospective analysis of data from 13 completed randomised trials in patients with various tumour types, 3 patients out of 91 (3.3%) with brain metastases experienced CNS bleeding (all Grade 4) when treated with Altuzan, compared to 1 case (Grade 5) out of 96 patients (1%) that were not exposed to Altuzan. In two subsequent studies in patients with treated brain metastases (which included around 800 patients), one case of Grade 2 CNS haemorrhage was reported.
Intracranial haemorrhage can occur in patients with relapsed glioblastoma. In study AVF3708g, CNS haemorrhage was reported in 2.4% (2/84) of patients in the Altuzan alone arm (Grade 1); and in 3.8% (3/79) of patients treated with Altuzan and irinotecan (Grades 1, 2 and 4).
Across all Altuzan clinical trials, mucocutaneous haemorrhages were seen in up to 50% of patients treated with Altuzan. These were most commonly NCI-CTC grade 1 epistaxis that lasted less than 5 minutes, resolved without medical intervention and did not require any change in the Altuzan treatment regimen. Clinical safety data suggest that the incidence of minor mucocutaneous haemorrhage (eg, epistaxis) may be dose-dependent.
There have also been less common events of minor mucocutaneous haemorrhage in other locations such as, gingival bleeding or vaginal bleeding.
Hypertension : An increased incidence of hypertension (all grades) of up to 42.1% has been observed in patients treated with Altuzan compared with up to 14% in the comparator arm. In clinical trials across all indications, the overall incidence of NCI-CTC grade 3 and 4 hypertension in patients receiving Altuzan ranged from 0.4 to 17.9%. Grade 4 hypertension (hypertensive crisis) occurred in up to 1% of patients treated with Altuzan compared to up to 0.2% patients treated with the same chemotherapy alone.
Hypertension was generally adequately controlled with oral antihypertensives such as, angiotensin-converting enzyme inhibitors, diuretics and calcium-channel blockers. It rarely resulted in discontinuation of Altuzan treatment or hospitalisation.
Very rare cases of hypertensive encephalopathy have been reported, some of which were fatal. The risk of Altuzan-associated hypertension did not correlate with the patients' baseline characteristics, underlying disease or concomitant therapy.
Posterior Reversible Encephalopathy Syndrome : Two confirmed cases (0.8%) of PRES have been reported in one clinical study. Symptoms usually resolve or improve within days, although some patients have experienced neurologic sequelae.
Thromboembolism: Arterial Thromboembolism: An increased incidence of arterial thromboembolic events was observed in patients treated with Altuzan across indications including cerebrovascular accidents, myocardial infarction, transient ischemic attacks, and other arterial thromboembolic events.
In clinical trials, the overall incidence ranged up to 5.9% in the Altuzan-containing arms compared up to 1.7% in the chemotherapy control arms. Fatal outcome was reported in 0.8% of patients receiving Altuzan in combination with chemotherapy compared to 0.5% of patients receiving chemotherapy alone. Cerebrovascular accidents (including transient ischemic attacks) were reported in up to 2.3% of Altuzan-treated patients versus 0.5% of patients in the control group. Myocardial infarction was reported in 1.4% of Altuzan treated versus 0.7% of patients in the observed control group.
In one clinical trial, AVF2192g, patients with metastatic colorectal cancer who were not candidates for treatment with irinotecan, were included. In this trial, arterial thromboembolic events were observed in 11% (11/100) of Altuzan patients compared to 5.8% (6/104) in the chemotherapy-control group. In an uncontrolled clinical trial, AVF3708g, in patients with relapsed glioblastoma, arterial thromboembolic events were observed in 6.3% (5/79) of patients who received Altuzan in combination with irinotecan compared to 4.8% (4/84) of patients who received Altuzan alone.
Venous Thromboembolism : In clinical trials across indications, the overall incidence of venous thromboembolic events ranged from 2.8 to 17.3% in the Altuzan-containing arms compared to 3.2 to 15.6% in the chemotherapy-control arms. Venous thromboembolic events include deep venous thrombosis and pulmonary embolism.
Grade 3-5 venous thromboembolic events have been reported in up to 7.8% of patients treated with chemotherapy plus Altuzan compared with up to 4.9% in patients with chemotherapy alone. Patients who have experienced a venous thromboembolic event may be at higher risk for a recurrence if they receive Altuzan in combination with chemotherapy versus chemotherapy alone.
From a clinical trial in patients with persistent, recurrent, or metastatic cervical cancer (study GOG-0240), grade 3-5 venous thromboembolic events have been reported in up to 10.6% of patients treated with chemotherapy and Altuzan compared with up to 5.4% in patients with chemotherapy alone.
In clinical trial BO21990, Grade 3-5 venous thromboembolic events were observed in 7.6% of patients with newly diagnosed glioblastoma treated with Altuzan in combination with chemotherapy and radiotherapy, compared to 8% of patients treated with chemotherapy and radiotherapy alone.
Congestive Heart Failure (CHF): In clinical trials with Altuzan, congestive heart failure (CHF) was observed in all cancer indications studied to date but occurred predominantly in patients with metastatic breast cancer. In 5 phase III studies (AVF2119g, E2100, BO17708 and AVF3694g and AVF3693g) in patients with metastatic breast cancer, CHF grade 3 or higher, was reported in up to 3.5% of patients treated with Altuzan in combination with chemotherapy compared with up to 0.9% in the control arms. For patients in study AVF3694g who received anthracyclines concomitantly with Altuzan, the incidences of grade 3 or higher CHF for the respective Altuzan and control arms were similar to those in the other studies in metastatic breast cancer: 2.9% in the anthracycline+Altuzan arm and 0% in the anthracycline+placebo arm. In addition, in study AVF3694g, the incidences of all grade CHF were similar between the anthracycline+Altuzan (6.2%) and the anthracycline+placebo arms (6%).
Most patients who developed CHF during mBC trials showed improved symptoms and/or left ventricular function following appropriate medical therapy.
In most clinical trials of Altuzan, patients with pre-existing CHF of NYHA II-IV were excluded, therefore, no information is available on the risk of CHF in this population.
Prior anthracyclines exposure and/or prior radiation to the chest wall may be possible risk factors for the development of CHF.
An increased incidence of CHF has been observed in a clinical trial of patients with diffuse large B-cell lymphoma when receiving Altuzan with a cumulative doxorubicin dose greater than 300 mg/m2. This phase III clinical trial compared rituximab/cyclophosphamide/doxorubicin/vincristine/prednisone (R-CHOP) + Altuzan to R-CHOP without Altuzan. While the incidence of CHF was, in both arms, above that previously observed for doxorubicin therapy, the rate was higher in the R-CHOP + Altuzan arm.
Wound Healing : As Altuzan may adversely impact wound healing, patients who had major surgery within the last 28 days prior to starting Altuzan treatment were excluded from participation in phase III trials.
Across mCRC clinical trials, there was no increased risk of post-operative bleeding or wound healing complications observed in patients who underwent major surgery between 28-60 days prior to starting Altuzan therapy. An increased incidence of post-operative bleeding or wound healing complications occurring within 60 days of major surgery was observed, if the patient was being treated with Altuzan at the time of surgery. The incidence varied between 10% (4/40) and 20% (3/15).
Cases of serious wound healing complications have been reported during Altuzan use, some of which had a fatal outcome.
In locally recurrent and metastatic breast cancer trials, Grade 3-5 wound healing complications were observed in up to 1.1% of patients receiving Altuzan compared with up to 0.9% of patients in the control arms.
In a study of patients with relapsed glioblastoma (study AVF3708g), the incidence of postoperative wound healing complications (including craniotomy site wound dehiscence and cerebrospinal fluid leak) was 3.6% in patients treated with single-agent Altuzan and 1.3% in patients treated with Altuzan plus irinotecan.
In patients with newly diagnosed glioblastoma (study BO21990) the incidence of grade 3-5 postoperative wound healing complications (including complications following craniotomy) was 3.3% when treated with Altuzan in combination with chemotherapy and radiotherapy, compared with 1.6% when treated with chemotherapy and radiotherapy alone.
Proteinuria : In clinical trials, proteinuria has been reported within the range of 0.7 to 38% of patients receiving Altuzan. Proteinuria ranged in severity from clinically asymptomatic, transient, trace proteinuria to nephrotic syndrome. Grade 3 proteinuria was reported in up to 8.1% of treated patients, grade 4 proteinuria (nephrotic syndrome) was seen in up to 1.4% of treated patients. The proteinuria seen in Altuzan clinical trials was not associated with renal impairment and rarely required permanent discontinuation of Altuzan therapy.
Patients with a history of hypertension may be at increased risk for the development of proteinuria when treated with Altuzan. There is evidence suggesting that grade 1 proteinuria may be related to Altuzan dose. Testing for proteinuria is recommended prior to start of Altuzan therapy. In most clinical studies, urine protein levels of ≥2 g/24 hrs led to the holding of Altuzan until recovery to <2 g/24 hrs.
Hypersensitivity and Infusion Reactions : In some clinical trials, anaphylactic and anaphylactoid-type reactions were reported more frequently in patients receiving Altuzan in combination with chemotherapies than with chemotherapy alone. The incidence of these reactions in some clinical trials of Altuzan is common (up to 5% in Altuzan-treated patients).
Ovarian Failure/Fertility : The incidence of new cases of ovarian failure, defined as amenorrhoea lasting 3 or more months, FSH level ≥30 mIU/mL and a negative serum β-HCG pregnancy test, has been evaluated. New cases of ovarian failure were reported more frequently in patients receiving Altuzan. After discontinuation of Altuzan treatment, ovarian function recovered in a majority of women. Long-term effects of the treatment with Altuzan on fertility are unknown.
Infections : In clinical trial BO21990, a randomised, double-blind, placebo controlled, multicentre phase III study of Altuzan in combination with chemotherapy plus radiotherapy for the treatment of patients with newly diagnosed glioblastoma, the incidence of all grade and grade 3-5 infections was 54.4% and 12.8% in the Altuzan plus chemotherapy and radiotherapy arm versus 39.1% and 7.8% in the chemotherapy plus radiotherapy only arm, respectively.
Elderly Patients: In randomised clinical trials, >65 years was associated with an increased risk of developing arterial thromboembolic events including cerebrovascular accidents, transient ischemic attacks and myocardial infarction as compared to those ≤65 years when treated with Altuzan.
Other reactions with a higher frequency seen in patients over 65 were Grade 3-4 leucopenia and thrombocytopenia, and all grade neutropenia, diarrhoea, nausea, headache and fatigue.
From a clinical trial in patients with metastatic colorectal cancer (study AVF2107), no increase in the incidences of other reactions, including gastrointestinal perforation, wound healing complications, congestive heart failure and haemorrhage, was observed in elderly patients (>65 years) receiving Altuzan as compared to those ≤65 years treated with Altuzan.
Laboratory Abnormalities: Decreased neutrophil count, decreased white blood count and presence of urine protein may be associated with Altuzan treatment.
Across clinical trials, the following grade 3 and 4 laboratory abnormalities were seen with an increased (≥2%) incidence in patients treated with Altuzan compared to those in the control groups: Hyperglycaemia, decreased haemoglobin, hypokalaemia, hyponatraemia, decreased white blood cell count, increased prothrombin time (PT), normalised ratio.
ALTUZAN CONTRAINDICATIONS
See also:
What is the most important information I should know about Altuzan?
Treatment with Altuzan may cause you to have problems with wound healing, which could result in bleeding or infection. If you need to have any type of surgery, you will need to stop receiving Altuzan at least 4 weeks ahead of time. Do not start using Altuzan for at least 4 weeks after surgery, or until your surgical incision heals.
Before being treated with Altuzan, tell your doctor if you have a bleeding or blood-clotting disorder, heart disease, congestive heart failure, high blood pressure, or a history of heart attack, stroke, blood clots, or stomach or intestinal bleeding (including perforation).
Some people receiving a Altuzan injection have had a reaction to the infusion (when the medicine is injected into the vein). Tell your caregiver right away if you feel dizzy, nauseated, light-headed, sweaty, itchy, or have a fast heartbeat, chills, wheezing, or chest pain during the injection.
Call your doctor at once if you have: any unusual bleeding or bruising, blood in your urine or stools, coughing up blood, any bleeding that will not stop, severe stomach pain with fever and vomiting, sudden numbness or weakness, leg pain or swelling, chest pain, severe headache, problems with speech or balance, swelling or rapid weight gain, urinating less than usual, loss of bladder or bowel control, or missed menstrual periods.
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: