- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (197) +-
- Baby & Mom (1339) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3119) +-
- Beauty > Skin Care > whitening (309)
- Chemotherapy & Immune Response (885) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (290)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (191)
- HEMATOLOGY (39)
-
Medical Supplies (506)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (11)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (1)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2721)
+-
- Allergy & Sinus (95)
- Children's Health Care (54)
- Cough, Cold & Flu (281)
- Digestive Health & Nausea (231)
- Ear, Nose & Throat Care (179)
- Eye Care (124)
- Feminine Care (323)
- Foot Care (12)
- Orthopaedic Appliances (1)
- Pain Relief & Management (244)
- Pill Organizer (2)
- Skin Treatments (863)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3346)
+-
- Bath & Body (271)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (175)
- Eye Care (131)
- Feminine Care (372)
- Foot Care (20)
- Hair Care (503)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (26)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (64)
- Shaving & Grooming (75)
- Sun Care (80)
-
Prescription Drugs (2932)
+-
- Analgesics (184)
- Cardiovascular System (374)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (177)
- Gastrointestinal Tract (243)
- Gastrointestinal Tract > Hepatology > Liver treatment (60)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (47)
- NEUROLOGY (228)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (115)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (304) +-
- Vitamins & Minerals Supplements (1225) +-
Ex Tax: 1,100EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

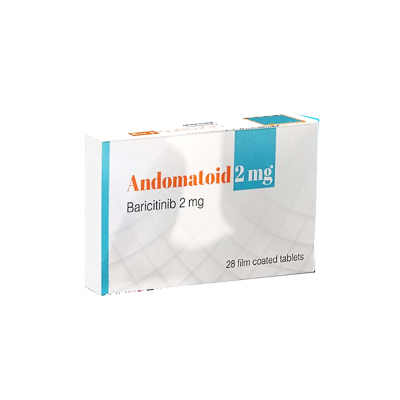
ANDOMATOID 2 MG ( BARICITINIB ) 28 FILM-COATED TABLETS
US Brand Name: Olumiant
Description
Baricitinib is used alone or together with other medicines (eg, methotrexate, DMARDs) to treat moderately to severely active rheumatoid arthritis in patients who have taken other medicines (eg, tumor necrosis factor or TNF antagonist) that did not work well.
Baricitinib is also used to treat coronavirus disease 2019 (COVID-19) in hospitalized patients requiring oxygen or assistance with breathing.
Baricitinib is also used to treat severe alopecia areata (autoimmune disorder that causes patchy hair loss).
Baricitinib is a Janus kinase (JAK) inhibitor that works on the immune system.
This medicine is available only with your doctor's prescription for rheumatoid arthritis. This medicine is to be given only by or under the immediate supervision of your doctor for COVID-19.
This product is available in the following dosage forms: Tablet
Before Using
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of baricitinib to treat rheumatoid arthritis and alopecia areata in children and to treat COVID-19 in children younger than 2 years of age. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of baricitinib in the elderly. However, elderly patients are more likely to have age-related kidney problems, which may require caution and adjustment in the dose for patients receiving baricitinib.
Breastfeeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abatacept
- Adalimumab
- Adenovirus Vaccine Type 4, Live
- Adenovirus Vaccine Type 7, Live
- Anakinra
- Bacillus of Calmette and Guerin Vaccine, Live
- Certolizumab Pegol
- Cholera Vaccine, Live
- Dengue Tetravalent Vaccine, Live
- Etanercept
- Fedratinib
- Fexinidazole
- Gemfibrozil
- Golimumab
- Guselkumab
- Infliximab
- Influenza Virus Vaccine, Live
- Ixekizumab
- Leflunomide
- Measles Virus Vaccine, Live
- Mumps Virus Vaccine, Live
- Nitisinone
- Poliovirus Vaccine, Live
- Probenecid
- Rituximab
- Rotavirus Vaccine, Live
- Rubella Virus Vaccine, Live
- Ruxolitinib
- Sarilumab
- Secukinumab
- Smallpox Monkeypox Vaccine
- Teriflunomide
- Tocilizumab
- Typhoid Vaccine, Live
- Upadacitinib
- Ustekinumab
- Vadadustat
- Varicella Virus Vaccine, Live
- Voriconazole
- Yellow Fever Vaccine
- Zoster Vaccine, Live
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Levothyroxine
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Anemia (blood disease) or
- Infection, history of or
- Neutropenia (blood disease) or
- Lymphopenia (blood disease) or
- Stomach or bowel problems (eg, blockage, diverticulitis, perforation, ulcers), history of—Use with caution. May make these conditions worse.
- Heart or blood vessel disease or
- Hepatitis B, history of or
- Hepatitis C, history of or
- Herpes zoster infection or
- Tuberculosis, history of or
- Weakened immune system—May cause side effects to become worse.
- Infection, active or
- Kidney disease, severe or
- Liver disease, severe or
- Tuberculosis, active—Use is not recommended in patients with these conditions.
- Kidney disease, moderate—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Smoker, current or past—May increase risk for serious side effects.
Proper Use
For COVID-19:
- A nurse or other trained health professional will give you this medicine in a medical facility. It is usually given once a day by mouth for up to 14 days or until you are discharged from the hospital (whichever comes first).
- This medicine comes with a Fact Sheet for Patients, Parents, and Caregivers. Read and follow the information in the Fact Sheet carefully. Ask your doctor if you have any questions.
For rheumatoid arthritis and alopecia areata: Use this medicine exactly as directed by your doctor. Do not take more or less of it, do not take it more often, and do not take it for a longer time than your doctor ordered.
This medicine comes with a Medication Guide and patient instructions. Read and follow these instructions carefully. Ask your doctor if you have any questions.
You may take this medicine with or without food.
Tell your doctor if you cannot swallow the tablet whole. The tablet can be mixed it in water and swallowed right away. It may also be given through a gastrostomy tube, nasogastric tube, or orogastric tube.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (tablets):
For alopecia areata:
- Adults—2 milligrams (mg) once a day. Your doctor may adjust your dose as needed.
- Children—Use and dose must be determined by your doctor.
For rheumatoid arthritis:
- Adults—2 milligrams (mg) once a day.
- Children—Use and dose must be determined by your doctor.
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions
It is very important that your doctor check your progress at regular visits. This will allow your doctor to see if this medicine is working properly and to decide whether you should continue to use it. Blood and urine tests are needed to check for unwanted effects.
You will need to have a skin test for tuberculosis before you start using this medicine. Tell your doctor if you or anyone in your home has ever had a positive reaction to a tuberculosis skin test.
Your body's ability to fight infections may be reduced while you are using baricitinib. It is very important that you call your doctor at the first sign of an infection. Check with your doctor right away if you have a fever, chills, cough, flu-like symptoms, or unusual tiredness or weakness.
This medicine may increase your risk of serious heart or blood vessel problems (eg, heart attack, stroke), especially in patients with rheumatoid arthritis who are 50 years of age and older and with a heart or blood vessel disease. Call your doctor right away if you have chest pain or discomfort, confusion, difficulty in speaking, double vision, headache, inability to move arms, legs, or facial muscles, nausea, pain or discomfort in the arms, jaw, back, or neck, sweating, trouble breathing, or vomiting.
This medicine may increase your risk of cancer (eg, lymphoma, lung cancer, non-melanoma skin cancer). Tell your doctor right away if you have black, tarry stools, general feeling of illness, swollen glands, weight loss, yellow skin and eyes, persistent non-healing sore, reddish patch or irritated area, shiny bump, pink growth, or white, yellow or waxy scar-like area on the skin.
This medicine may increase your risk of developing blood clots (eg, arterial thrombosis, deep vein thrombosis, pulmonary embolism), especially in patients with rheumatoid arthritis who are 50 years of age and older and with a heart or blood vessel disease. Check with your doctor right away if you have anxiety, chest pain, cough, dizziness, lightheadedness, or fainting, fast heartbeat, pain, redness, or swelling in the arm or leg, pains in the chest, groin, or legs, especially calves of the legs, severe headaches, sudden loss of coordination, sudden onset of slurred speech, sudden vision changes, or trouble breathing.
Baricitinib can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. If this occurs, there are certain precautions you can take, especially when your blood count is low, to reduce the risk of infection:
- If you can, avoid people with infections. Check with your doctor right away if you think you are getting an infection or if you get a fever or chills, cough or hoarseness, lower back or side pain, or painful or difficult urination.
- Check with your doctor right away if you notice any unusual bleeding or bruising, black, tarry stools, blood in the urine or stools, or pinpoint red spots on your skin.
- Be careful when using a regular toothbrush, dental floss, or toothpick. Your medical doctor, dentist, or nurse may recommend other ways to clean your teeth and gums. Check with your medical doctor before having any dental work done.
- Do not touch your eyes or the inside of your nose unless you have just washed your hands and have not touched anything else in the meantime.
- Be careful not to cut yourself when you are using sharp objects, such as a safety razor or fingernail or toenail cutters.
- Avoid contact sports or other situations where bruising or injury could occur.
While you are being treated with baricitinib, and after you stop treatment with it, do not have any immunizations (vaccines) without your doctor's approval. Baricitinib may lower your body's resistance and there is a chance you might get the infection the vaccine is meant to prevent. In addition, you should not be around other persons living in your household who receive live virus vaccines because there is a chance they could pass the virus on to you. Some examples of live vaccines include measles, mumps, influenza (nasal flu vaccine), poliovirus (oral form), rotavirus, and rubella. Do not get close to them and do not stay in the same room with them for very long. If you have questions about this, talk to your doctor.
This medicine can cause serious allergic reactions, including angioedema or urticaria. Tell your doctor right away if you start to have swelling of your face, lips, tongue, throat, arms, or legs, or if you are having trouble swallowing or breathing.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Side Effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Body aches or pain
- chest tightness
- chills
- cough
- difficulty in breathing
- ear congestion
- fever
- headache
- hoarseness
- loss of voice
- muscle aches
- pain or tenderness around the eyes and cheekbones
- runny or stuffy nose
- sneezing
- sore throat
- trouble in swallowing
- unusual tiredness or weakness
Less common
- Black, tarry stools
- bladder pain
- blemishes on the skin
- bloody or cloudy urine
- burning, itching, and pain in hairy areas, pus at the root of the hair
- chest pain or tightness
- cough producing mucus
- difficult, burning, or painful urination
- frequent urge to urinate
- itching of the vagina or outside genitals
- lower back or side pain
- pain, redness, or swelling in the arm or leg
- pain during sexual intercourse
- pains in the chest, groin, or legs, especially calves of the legs
- pale skin
- pimples
- severe headaches of sudden onset
- stomach pain
- sudden loss of coordination
- sudden onset of slurred speech
- sudden vision changes
- thick, white curd-like vaginal discharge without odor or with mild odor
- trouble breathing
- unusual bleeding or bruising
Rare
- Anxiety
- burning or stinging of the skin
- coughing or spitting up blood
- dizziness or lightheadedness
- increased weight
- night sweats
- painful blisters on the trunk of body
- painful cold sores or blisters on the lips, nose, eyes, or genitals
- sudden high fever or low-grade fever for months
Incidence not known
- Chest discomfort
- confusion
- difficulty in speaking
- double vision
- inability to move the arms, legs, or facial muscles
- inability to speak
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- nausea
- no blood pressure or pulse
- pain or discomfort in the arms, jaw, back or neck
- persistent non-healing sore
- pink growth
- reddish patch or irritated area
- shiny bump
- stopping of heart
- sweating
- unconsciousness
- white, yellow, or waxy scar-like area
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: