- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (192) +-
- Baby & Mom (1322) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3044) +-
- Beauty > Skin Care > whitening (307)
- Chemotherapy & Immune Response (883) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (289)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (192)
- HEMATOLOGY (39)
-
Medical Supplies (503)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (10)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (0)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2691)
+-
- Allergy & Sinus (95)
- Children's Health Care (54)
- Cough, Cold & Flu (277)
- Digestive Health & Nausea (233)
- Ear, Nose & Throat Care (179)
- Eye Care (124)
- Feminine Care (325)
- Foot Care (9)
- Orthopaedic Appliances (1)
- Pain Relief & Management (241)
- Pill Organizer (2)
- Skin Treatments (839)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3275)
+-
- Bath & Body (271)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (175)
- Eye Care (131)
- Feminine Care (374)
- Foot Care (17)
- Hair Care (472)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (22)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (65)
- Shaving & Grooming (65)
- Sun Care (80)
-
Prescription Drugs (2914)
+-
- Analgesics (181)
- Cardiovascular System (374)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (176)
- Gastrointestinal Tract (244)
- Gastrointestinal Tract > Hepatology > Liver treatment (62)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (46)
- NEUROLOGY (225)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (100)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (301) +-
- Vitamins & Minerals Supplements (1212) +-
Ex Tax: 6,091EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

MYFORTIC 360 MG ( MYCOPHENOLATE MOFETIL ) 120 FILM-COATED TABLETS
mycophenolate
Brand and Other Names:CellCept, Myfortic, MMF, Myhibbin
Dosage Forms & Strengths
capsule
250mg (generic; MMF)
tablet
500mg (generic, CellCept; MMF)
oral suspension
200mg/mL (generic, CellCept, Myhibbin; MMF)
powder for injection
500mg/vial (generic, CellCept; MMF)
tablet, delayed release (generic, Myfortic, MPA)
180mg
360mg
Kidney Transplant
Prophylaxis of organ rejection in patients receiving allogeneic renal transplants; use concomitantly with cyclosporine and corticosteroids
Mycophenolate mofetil (MMF): 1 g PO/IV q12hr, infused over ≥2 hours
Mycophenolic acid (MPA): 720 mg PO q12hr
Heart Transplant
Prophylaxis of organ rejection in patients receiving allogeneic cardiac transplants; use concomitantly with cyclosporine and corticosteroids
MMF: 1.5 g PO/IV q12hr, infused over ≥2 hours
Liver Transplant
Prophylaxis of organ rejection in patients receiving allogeneic hepatic transplants; use concomitantly with cyclosporine and corticosteroids
MMF (IV): 1 g q12hr; infused over ≥2 hours
MMF (PO): 1.5 g q12hr
Dosing Modifications
Renal impairment
- MMF: In severe renal impairment (glomerular filtration rate [GFR] <25 mL/min/1.73 m²), not to exceed 1 g q12hr
- No dosage adjustment needed in renal transplant patients experiencing delayed graft function postoperatively
Lupus Nephritis (Off-label)
Induction therapy for lupus nephritis (MMF)
Induction: 1 g PO q12hr with a glucocorticoid or 2-3 g for 6 months with glucocorticoids
Maintenance: 0.5-3 g/day or 1 g PO q12hr or 1-2 g daily
Administer with initial IV corticosteroid pulse for 3 days, then prednisone 0.5-1 mg/kg/day PO; not to exceed 10 mg/day; after a few weeks, prednisone may be tapered to lowest effective dose
Interactions
All InteractionsSort By:
Severity
Contraindicated (2)
- cholestyramine
- colestipol
Serious (82)
- adalimumab
- adenovirus types 4 and 7 live, oral
- alefacept
- amoxicillin
- ampicillin
- anakinra
- anthrax vaccine
- antithymocyte globulin equine
- antithymocyte globulin rabbit
- axicabtagene ciloleucel
- azathioprine
- basiliximab
- BCG vaccine live
- brexucabtagene autoleucel
- canakinumab
- carbonyl iron
- ciltacabtagene autoleucel
- diphtheria & tetanus toxoids
- diphtheria & tetanus toxoids/ acellular pertussis vaccine
- diphtheria & tetanus toxoids/acellular pertussis/poliovirus, inactivated vaccine
- etanercept
- ethinylestradiol
- etrasimod
- everolimus
- ferric maltol
- ferrous fumarate
- ferrous gluconate
- ferrous sulfate
- glatiramer
- golimumab
- hepatitis A vaccine inactivated
- hepatitis a/b vaccine
- hepatitis a/typhoid vaccine
- hepatitis b vaccine
- human papillomavirus vaccine, nonavalent
- hydroxychloroquine sulfate
- idecabtagene vicleucel
- infliximab
- influenza virus vaccine quadrivalent
- influenza virus vaccine quadrivalent, adjuvanted
- influenza virus vaccine quadrivalent, cell-cultured
- influenza virus vaccine quadrivalent, intranasal
- influenza virus vaccine trivalent
- influenza virus vaccine trivalent, adjuvanted
- influenza virus vaccine trivalent, intranasal
- iron dextran complex
- iron sucrose
- Japanese encephalitis virus vaccine
- leflunomide
- lisocabtagene maraleucel
- measles mumps and rubella vaccine, live
- measles, mumps, rubella and varicella vaccine, live
- meningococcal A C Y and W-135 polysaccharide vaccine combined
- muromonab CD3
- nafcillin
- pneumococcal vaccine 13-valent
- pneumococcal vaccine polyvalent
- polysaccharide iron
- rabies vaccine
- rabies vaccine chick embryo cell derived
- rilonacept
- rose hips
- rotavirus oral vaccine, live
- sirolimus
- smallpox and mpox (vaccinia) vaccine, live
- tacrolimus
- temocillin
- temsirolimus
- tetanus toxoid adsorbed or fluid
- tick-borne encephalitis vaccine
- tisagenlecleucel
- tocilizumab
- tofacitinib
- tongkat ali
- travelers diarrhea and cholera vaccine inactivated
- typhoid polysaccharide vaccine
- typhoid vaccine live
- upadacitinib
- ustekinumab
- varicella virus vaccine live
- yellow fever vaccine
- zoster vaccine live
Monitor Closely (111)
- aceclofenac
- acemetacin
- acyclovir
- aluminum hydroxide
- aminohippurate sodium
- aspirin
- aspirin rectal
- aspirin/citric acid/sodium bicarbonate
- astragalus
- balsalazide
- belatacept
- bendroflumethiazide
- calcium carbonate
- cefadroxil
- cefamandole
- cefpirome
- ceftibuten
- celecoxib
- cephalexin
- chlorothiazide
- chlorthalidone
- cholera vaccine
- choline magnesium trisalicylate
- cyclopenthiazide
- cyclosporine
- dengue vaccine
- denosumab
- dexlansoprazole
- dichlorphenamide
- diclofenac
- dicloxacillin
- didanosine
- diflunisal
- echinacea
- esomeprazole
- etodolac
- famotidine
- fenoprofen
- fingolimod
- flurbiprofen
- ganciclovir
- haemophilus influenzae type b vaccine
- hydrochlorothiazide
- hydroxyurea
- ibuprofen
- ibuprofen IV
- ibuprofen/famotidine
- indapamide
- indomethacin
- influenza virus vaccine quadrivalent, recombinant
- influenza virus vaccine trivalent, recombinant
- isavuconazonium sulfate
- ketoprofen
- ketorolac
- ketorolac intranasal
- lansoprazole
- levoketoconazole
- levonorgestrel oral
- lomustine
- lornoxicam
- magnesium supplement
- maitake
- mechlorethamine
- meclofenamate
- mefenamic acid
- meloxicam
- meningococcal group B vaccine
- mercaptopurine
- mesalamine
- methotrexate
- methyclothiazide
- metolazone
- nabumetone
- naproxen
- nizatidine
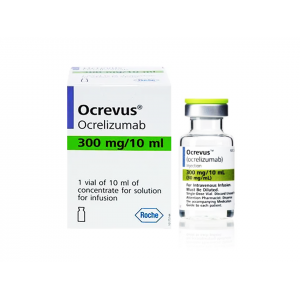
- ocrelizumab
- ocrelizumab/hyaluronidase
- ofatumumab SC
- olaparib
- omeprazole
- oxaprozin
- ozanimod
- pantoprazole
- parecoxib
- patiromer
- piroxicam
- poliovirus vaccine inactivated
- ponesimod
- probenecid
- rabeprazole
- rose hips
- salicylates (non-asa)
- salsalate
- siponimod
- sipuleucel-T
- sodium bicarbonate
- sodium citrate/citric acid
- sodium zirconium cyclosilicate
- sulfasalazine
- sulindac
- telmisartan
- tolfenamic acid
- tolmetin
- trastuzumab
- trastuzumab deruxtecan
- ublituximab
- valganciclovir
- vonoprazan
- willow bark
- xanomeline/trospium
- zoster vaccine recombinant
Minor (10)
- bazedoxifene/conjugated estrogens
- conjugated estrogens
- conjugated estrogens, vaginal
- estradiol
- estrogens conjugated synthetic
- estrogens esterified
- estropipate
- mestranol
- nirmatrelvir/ritonavir
- phenytoin
Adverse Effects
>10%
- Hyperglycemia (44%)
- Hypercholesterolemia (41%)
- Hypomagnesemia (39%)
- Dyspnea (37%)
- Back pain (35%)
- Increased blood urea nitrogen (BUN) (35%)
- Leukopenia (34%)
- Pleural effusion (34%)
- Urinary tract infection (34%)
- Increasing frequency of cough (31%)
- Hypocalcemia (30%)
- Hypertension (28%)
- Abdominal pain (27%)
- Peripheral edema (27%)
- Anemia (26%)
- Fever (23%)
- Nausea (23%)
- Hyperkalemia (22%)
- Diarrhea (21%)
- Infection (21%)
- Headache (16%)
1-10%
- Melanoma (1.6-4.2%)
- Other malignancies (0.7-2.1%)
- Lymphoma (0.4-1%)
- Opportunistic infection (including herpes)
- Neutropenia
- GI bleeding
- Pulmonary fibrosis
- Progressive multifocal leukoencephalopathy
Postmarketing Reports
BK virus-associated nephropathy
Congenital malformations, including ear, facial, cardiac and nervous system malformations and an increased incidence of first-trimester pregnancy
Colitis (sometimes caused by cytomegalovirus), pancreatitis, isolated cases of intestinal villous atrophy
Cases of pure red cell aplasia (PRCA) and hypogammaglobulinemia reported when administered in combination with other immunosuppressive agents
Cardiovascular: Venous thrombosis when therapy administered intravenously
Hematologic and lymphatic: Bone marrow failure, cases of pure red cell aplasia (PRCA)
Immune: Hypersensitivity, acute inflammatory syndrome resulting from de novo purine synthesis inhibitors
Infections: Bronchiectasis, interstitial lung disease
Vascular: Lymphocele
Warnings
|
Black Box Warnings Drug should be prescribed only by healthcare providers experienced in immunosuppressive therapy and management of renal, cardiac, or hepatic transplant patients Patients receiving drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources Drug increases risk of developing lymphoma and risk of skin malignancy Increased susceptibility to bacterial, viral, fungal and protozoal infections, including opportunistic infections and viral reactivation of hepatitis B and C, which may lead to hospitalizations and fatal outcomes Myfortic and CellCept dosage form absorbed differently; not for use interchangeably Healthcare provider responsible for maintenance therapy should have all information required for follow-up Risk of first-trimester miscarriage and congenital malformations; avoid if safer treatment options are available; females of reproductive potential must be counseled regarding pregnancy prevention and planning; after negative pregnancy test and follow-up, women of child-bearing age should use 2 forms of reliable contraception (hormone plus barrier) during entire course of mycophenolate therapy and continue until 6 weeks after drug discontinuance |
Contraindications
Hypersensitivity
IV formulation (CellCept) in patients allergic to polysorbate 80
Cautions
Pure red-cell aplasia reported in patients treated with MMF or MPA in combination with other immunosuppressive agents
Avoid use in hypoxanthine-guanine phosphoribosyltransferase (HGPRT) deficiency (Lesch-Nyhan, Kelley-Seegmiller syndrome)
Risk of miscarriage and congenital malformations, especially external ear and other facial abnormalities including cleft lip and palate, and anomalies of the distal limbs, heart, esophagus, kidney and nervous system (see Black Box Warnings); females of reproductive potential must be made aware of risks and must be counseled regarding pregnancy prevention and planning; avoid use of MMF during pregnancy if safer treatment options are available
Drug increases risk of developing lymphoma; risk appears to be related to intensity and duration of immunosuppression rather than to use of any specific agent; for patients with increased risk for skin cancer, exposure to sunlight and UV light should be limited by wearing protective clothing and using a broad-spectrum sunscreen with a high protection factor
MPA not indicated for hepatic or cardiac transplants
Use may be rarely associated with gastric or duodenal ulcers, GI bleeding and/or perforation
Safety and effectiveness of MPA for de novo pediatric renal transplant not established
Neutropenia may occur (may require dose reduction)
Must not be administered by rapid or bolus IV injection; increases risk of local adverse reactions such as phlebitis and thrombosis
Toxicity may increase in renal impairment; use caution
Patients should not donate blood during therapy and for at least 6 weeks following discontinuation of therapy because their blood or blood products might be administered to a female of reproductive potential or a pregnant woman
Based on animal data, men should not donate semen during therapy and for 90 days following discontinuation of drug Phenylalanine can be harmful to patients with phenylketonuria (PKU)
Immunosuppression increases risk of developing lymphoma and skin malignancies; majority of post-transplant lymphoproliferative disorder (PTLD) cases appear to be related to Epstein Barr Virus (EBV) infection; the risk of PTLD appears greatest in those individuals who are EBV seronegative, a population which includes many young children
A variety of drugs have potential to alter systemic MPA exposure when co-administered with this drug; determination of mycophenolic acid (MPA) concentrations in plasma before and after making any changes to immunosuppressive therapy, or when adding or discontinuing concomitant medications, may be appropriate to ensure MPA concentrations remain stable
Therapy may impact ability to drive and use machines; patients should avoid driving or using machines if they experience somnolence, confusion, dizziness, tremor, or hypotension during treatment
Oral suspension dosage form contains aspartame, a source of phenylalanine (0.56 mg phenylalanine/mL suspension); before prescribing oral suspension to a patient with PKU, consider combined daily amount of phenylalanine from all sources, including drug
Use of live attenuated vaccines should be avoided (eg, intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines) and patients should be advised that vaccinations may be less effective; advise patients to discuss with physician before seeking any immunizations
Acute inflammatory syndrome
- Acute inflammatory syndrome (AIS) reported with the use of MMF and mycophenolate products, and some cases have resulted in hospitalization
- AIS is a paradoxical pro-inflammatory reaction characterized by fever, arthralgias, arthritis, muscle pain, and elevated inflammatory markers including, C-reactive protein and erythrocyte sedimentation rate, without evidence of infection or underlying disease recurrence
- Symptoms occur within weeks to months of initiation of treatment or a dose increase; after discontinuation, improvement of symptoms and inflammatory markers are usually observed within 24 to 48 hours
- Monitor patients for symptoms and laboratory parameters of AIS when starting treatment with mycophenolate products or when increasing the dosage
- Discontinue treatment and consider other treatment alternatives based on risk and benefit for the patient
Serious infections and viral reactivation
- Risk of infection increases with total immunosuppressive load
- Increased risk of developing bacterial, fungal, protozoal, and new or reactivated viral infections, including opportunistic infections
- Because of danger of over suppression of immune system, which can increase susceptibility to infection, combination immunosuppressant therapy should be used with caution
- May increase risk of new or reactivated viral infections, including polyomavirus-associated nephropathy (PVAN), JC virus-associated progressive multifocal leukoencephalopathy (PML), cytomegalovirus (CMV) infections, reactivation of hepatitis B or C, SARS- CoV-2 infection
- PVAN, especially when due to BK virus infection, is associated with serious outcomes, including deteriorating renal function and renal graft loss
- PML, which is sometimes fatal, typically presents with hemiparesis, apathy, confusion, cognitive deficiencies, and ataxia
- Consider dose reduction or discontinuation in patients who develop new infections or reactivate viral infections, weighing the risk that reduced immunosuppression represents to the functioning allograft
Pregnancy & Lactation
Pregnancy
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to mycophenolate during pregnancy and those becoming pregnant within 6 weeks of discontinuing therapy; to report pregnancy or obtain information about the registry, visit www.mycophenolateREMS.com or call 1-800-617-8191
Use of mycophenolate mofetil (MMF) during pregnancy is associated with an increased risk of first-trimester pregnancy loss and an increased risk of multiple congenital malformations in multiple organ systems
Consider alternative immunosuppressants with less potential for embryofetal toxicity; risks and benefits of therapy should be discussed with the pregnant woman; the estimated background risk of pregnancy loss and congenital malformations in organ transplant populations is not clear
Animal data
- In animal reproductive toxicology studies, there were increased rates of fetal resorptions and malformations in absence of maternal toxicity
- Oral administration of MMF to pregnant rats from gestational day 7 to day 16 produced increased embryofetal lethality and fetal malformations including anophthalmia, agnathia, and hydrocephaly at doses equivalent to 0.015 and 0.01 times the recommended human doses for renal and cardiac transplant patients, respectively, when corrected for BSA
- Oral administration of MMF to pregnant rabbits from gestational Day 7 to Day 19 produced increased embryofetal lethality and fetal malformations included ectopia cordis, ectopic kidneys, diaphragmatic hernia, and umbilical hernia at dose equivalents as low as 0.05 and 0.03 times recommended human doses for renal and cardiac transplant patients, respectively, when corrected for BSA
- Females and males of reproductive potential
- Genotoxic effects have been observed in animal studies at exposures exceeding human therapeutic exposures by approximately 1.25 times; risk of genotoxic effects on sperm cells cannot be excluded
- Based on potential risk, sexually active male patients and/or their female partners are recommended to use effective contraception during treatment of male patient and for at least 90 days after cessation of treatment; also, based on potential risk of genotoxic effects, male patients should not donate sperm during treatment with this medication and for at least 90 days after cessation of treatment
Lactation
There are no data on presence of drug in human milk, or effects on milk production; there are limited data in the National Transplantation Pregnancy Registry on effects of mycophenolate on a breastfed child; studies in rats treated with MMF have shown mycophenolic acid (MPA) to be present in milk
Because available data are limited, it is not possible to exclude potential risks to a breastfeeding infant; the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for therapy and any potential adverse effects on breastfed infant from drug or from the underlying maternal condition
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk.
C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done.
D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk.
X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist.
NA: Information not available.
Pharmacology
Mechanism of Action
Inhibits T- and B-cell proliferation, as well as antibody production
Acts as noncompetitive, selective, and reversible inhibitor of inosine monophosphate dehydrogenase (IMPDH)
Absorption
Bioavailability: 94% (CellCept); 72% (Myfortic)
Peak plasma time: 1.5 hr
Distribution
Protein bound: 82-97%
Vd (MMF): IV, 3.6 L/kg; PO, 4.0 L/kg
Vd (MPA): Steady state, 54 L; elimination phase, 112 L
Metabolism
Metabolized via enterohepatic recirculation
Metabolites: MPA (active form; MMF is prodrug)
Elimination
Half-life (MMF): PO, 18 hr; IV, 17 hr
Half-life (MPA): PO, 8-16 hr; MPA glucuronide (MPAG), 13-17 hr
Excretion as metabolites: Urine; feces
Administration
Preparation
Teratogenicity
- Teratogenic effects demonstrated in humans; follow applicable special handling and disposal procedures
- Avoid inhalation or direct contact with skin or mucous membranes of the dry powder or the constituted suspension
- Wear disposable gloves during reconstitution and when wiping outer surface of bottle/cap and table surface after reconstitution
- If such contact occurs, wash hands thoroughly with soap and water; rinse eyes with water
Oral suspension
- Measure 94 mL of water in graduated cylinder
- Add ~50% of total amount of water for reconstitution to bottle and shake closed bottle well for ~1 minute
- Add remaining water, close bottle, and shake well for ~1 minute
- Remove child-resistant cap and push bottle adapter into neck of bottle
- Close bottle with child-resistant cap tightly; this will assure proper seating of bottle adapter in bottle and child-resistant status of cap
- Write expiration date of constituted suspension on the bottle label (shelf-life of constituted suspension is 60 days
- Dispense with “Instruction for Use” and oral dispensers
- Alert patients to read important handling information described
IV
- Does not contain antibacterial preservative; therefore, reconstitution and dilution must be done aseptically in vertical laminar flow hood, with same precautions as for antineoplastic agents
- Step 1
- To prepare 1-g dose, use 2 vials; to prepare 1.5-g dose, use 3 vials
- Reconstitute contents of each vial by injecting 14 mL D5W, then gently shake to dissolve
- Before diluting further, inspect resulting slightly yellow solution for particulate matter and discoloration; discard if either is observed
- Step 2
- To prepare 1-g dose, further dilute contents of 2 reconstituted vials into 140 mL D5W; to prepare 1.5-g dose, further dilute contents of 3 reconstituted vials into 210 mL D5W; final concentration of both solutions is 6 mg/mL
- Inspect infusion solution for particulate matter and discoloration; discard if either is observed
Oral Administration
- Take on empty stomach 1 hour before or 2 hours after meals
- Once dosage is stabilized, MMF can be taken with food after kidney transplant
- Solid PO forms: Swallow whole; do not chewed, crush, or split; do not open capsules
IV Administration
- IV recommended for patients unable to take oral
- IV and PO doses are equivalent to one another
- May be administered for up to 14 days; however, switch patient to PO as soon as they can tolerate oral medication
- Infuse over ≥2 hours
- Do not administer via rapid or bolus injection
Storage
IV
- Infusion solution is stable for 4 hr after reconstitution and dilution
- Store powder or solution at 15-30°C (59-86°F)
PO
Capsules/tablets
- Store at 25ºC (77ºF); excursions permitted to 15-30°C (59-86°F)
- Dispense in light-resistant containers, such as the manufacturer’s original containers
Powder
- Store at 25ºC (77ºF); excursions permitted to 15-30°C (59-86°F)
Reconstituted PO suspension
- Store at 25ºC (77ºF); excursions permitted to 15-30°C (59-86°F), OR
- Refrigerate at 2-8ºC (36-46ºF)
- Do not freeze
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: