- Anti-hestaminic & Respiratory Drugs (20)
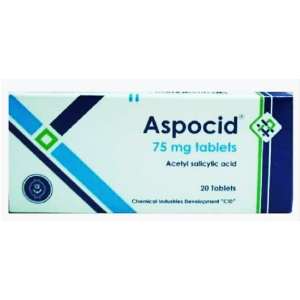
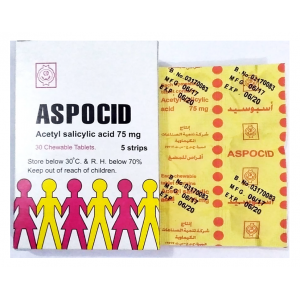
- Anti-inflammatory Drugs (192) +-
- Baby & Mom (1319) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3008) +-
- Beauty > Skin Care > whitening (299)
- Chemotherapy & Immune Response (882) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (289)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (281) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (191)
- HEMATOLOGY (39)
-
Medical Supplies (503)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (10)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (0)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2644)
+-
- Allergy & Sinus (95)
- Children's Health Care (54)
- Cough, Cold & Flu (277)
- Digestive Health & Nausea (225)
- Ear, Nose & Throat Care (179)
- Eye Care (117)
- Feminine Care (325)
- Foot Care (9)
- Orthopaedic Appliances (0)
- Pain Relief & Management (237)
- Pill Organizer (2)
- Skin Treatments (817)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3257)
+-
- Bath & Body (271)
- Deodorant & Anti-perspirants (190)
- Ear, Nose & Throat Care (175)
- Eye Care (124)
- Feminine Care (374)
- Foot Care (17)
- Hair Care (472)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (22)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (88)
- Pregnancy & Fertility (64)
- Shaving & Grooming (65)
- Sun Care (79)
-
Prescription Drugs (2882)
+-
- Analgesics (181)
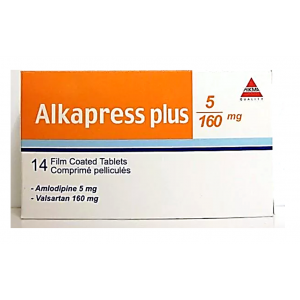
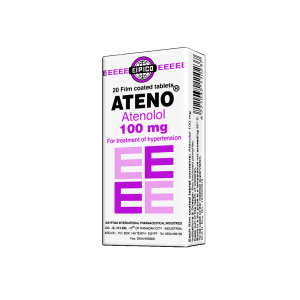
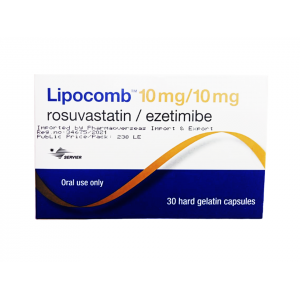
- Cardiovascular System (374)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (176)
- Gastrointestinal Tract (242)
- Gastrointestinal Tract > Hepatology > Liver treatment (61)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (46)
- NEUROLOGY (222)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (80)
- Vaccines (1)
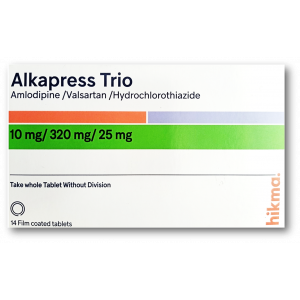
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (301) +-
- Vitamins & Minerals Supplements (1203) +-
Ex Tax: 46EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

Altiazem 60 mg ( Diltiazem hydrochloride ) 40 modified-release MR tablets
Prescription Information
Composition
Each MR tablet contains:
Diltiazem hydrochloride ........................................................................................ 60 mg
Inactive ingredients:
Lactose, hydrogenated castor oil, polyethylene glycol 6000, magnesium stearate.
Therapeutic Indications
Prophylaxis and treatment of angina pectoris.
Treatment of mild to moderate arterial hypertension.
Dosage and Administration
ALTIAZEM Tablets should be swallowed whole with some water, without crushing or chewing.
Angina pectoris:
Adults:
The usual dose is one tablet (60 mg) three times daily.
However, patient responses may vary and dosage requirements can differ significantly between individual patients.
If necessary the dosage may be increased, up to 360 mg/day.
Higher doses, up to 480 mg/day, have been used with benefit in some patients, especially in the treatment of unstable angina.
Mild to moderate arterial hypertension:
Half tablet (30 mg) three times daily.
Elderly patients or patients with impaired hepatic or renal function:
Plasma levels of diltiazem can be increased in these patients. The recommended initial dose is half tablet (30 mg) three times daily. Heart rate should be monitored regularly in these patients and the dose should not be increased if the heart rate falls below 50 beats per minute. In patients suffering from liver problems, periodical checks of liver function are recommended during treatment with ALTIAZEM 60 mg MR Tablet.
Children:
Not recommended.
Contraindications
Congestive heart failure, sick sinus syndrome [sinoatrial (SA) and 2nd or 3rd degree atrioventricular (AV) block] in patients without a functioning pacemaker, marked bradycardia (less than 50 beats per minute).
ALTIAZEM should not be used in pregnancy, in women of child-bearing potential or in mothers who are breastfeeding.
Left ventricular failure with pulmonary stasis.
Hypersensitivity to diltiazem or to any of its excipients.
ALTIAZEM like any calcium-channel blocker should not be administered concurrently with dantrolene infusion, because of the risk of ventricular fibrillation (see Drug Interactions).
ALTIAZEM contains lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose galactose malabsorption should not take this medicine.
Warnings and Precautions
ALTIAZEM should be used with caution in patients with reduced left ventricular function, mild bradycardia (because of risk of exacerbation), first degree AV block or prolonged PR interval detected on electrocardiogram (risk of exacerbation and rarely, of complete block).
In case of surgery with general anaesthesia inform anaesthetist about current therapy and dosage. Calcium channel blockers may potentiate the depression of cardiac contractility, conductivity and automaticity and vascular dilatation caused by anaesthetics.
The product should be used with caution in elderly patients and in patients with hepatic and renal dysfunction, since plasma diltiazem levels can be increased.
The contraindications and precautions should be carefully observed and close monitoring, particularly of heart rate, should be carried out at the beginning of treatment.
Drug Interactions
Combinations contraindicated:
Dantrolene (infusion):
Lethal ventricular fibrillation is regularly observed in animals when intravenous verapamil and dantrolene are administered concomitantly. The combination of a calcium antagonist and dantrolene is therefore potentially dangerous (see Contraindications).
Combinations requiring caution:
In common with other calcium-channel blockers, when ALTIAZEM is used with drugs which may induce bradycardia or hypotension or with other antiarrhythmic drugs the possibility of an additive effect should be borne in mind.
Alpha-antagonist agents:
Increase of hypotensive effect. Combination of diltiazem with alpha-antagonist drugs may produce or aggravate hypotension; therefore strict monitoring is recommended.
Beta-blockers:
Possible disturbances of conduction (marked bradycardia, sinus node depression), effects on sinoatrial and atrioventricular conduction and heart failure (synergistic action). Patients receiving such combinations should be regularly monitored by ECG and clinically, especially when initiating the treatment.
Amiodarone, digoxin:
Increased risk of bradycardia; caution required in combination with diltiazem, especially in elderly patients, or at high dosages. Diltiazem increases blood levels of digoxin.
Antiarrhythmic drugs:
Since diltiazem has antiarrhythmic activity, concurrent prescription of other antiarrhythmic agents may result in increase of cardiac side effects due to additive effects. Such a combination requires caution and it should be initiated under close ECG and clinical monitoring.
Nitro-compounds:
Should be prescribed at gradually increasing doses because of increase in hypotensive effects and faintness from the additive effects on vasodilation.
Ciclosporin, Tacrolimus and Sirolimus:
Diltiazem causes an increase of blood levels. It is recommended to decrease the dose, check renal function, titrate blood levels and adjust the dose of both during the treatment combination and after its discontinuation.
Carbamazepine:
Increase of blood levels of carbamazepine. It is recommended that the plasma concentration of carbamazepine be monitored and the dose adjusted as necessary.
Theophylline:
Increase of blood levels of theophylline.
Histamine H2-receptor antagonists (cimetidine or ranitidine):
Increase of plasma levels of diltiazem. Patients currently receiving ALTIAZEM therapy should be carefully monitored when initiating or discontinuing therapy with anti-H2 agents. A change in the diltiazem dose may be necessary.
Rifampicin:
Plasma levels of diltiazem may be decreased after beginning rifampicin. The patient should be carefully monitored when initiating or discontinuing rifampicin treatment.
Lithium:
Risk of lithium-induced neurotoxicity.
Combinations to be taken into account:
CYP450 3A4:
Diltiazem can affect plasma levels of drugs metabolised exclusively via CYP450 3A4. The concomitant therapy of diltiazem and drugs metabolised via CYP450 3A4 may increase the risk of adverse reactions.
Statins:
Diltiazem is an inhibitor of CYP3A4 and has been shown to significantly increase the AUC of some statins. The risk of myopathy and rhabdomyolysis is increased by concomitant administration of diltiazem with statins metabolised by CYP3A4 (e.g. atorvastatin, fluvastatin and simvastatin). An adjustment to the dose of statin may be necessary (see also product information of the relevant statin). When possible, it is recommended to use a statin not metabolised by CYPA4 (e.g. pravastatin) with diltiazem.
Benzodiazepines (midazolam, triazolam):
Diltiazem significantly increases plasma concentrations of midazolam and triazolam and prolongs their half-life. Special care should be taken when prescribing short-acting benzodiazepines metabolised by the CYP3A4 pathway in patients using diltiazem.
Corticosteroids (methylprednisolone):
Diltiazem can increase methylprednisolone levels (through inhibition of CYP3A4 and possible inhibition of P-glycoprotein). The patient should be monitored when initiating methylprednisolone treatment. An adjustment to the dose of methylprednisolone may be necessary.
General information to be taken into account:
Due to the potential for additive effects, caution and careful titration are necessary in patients receiving diltiazem concomitantly with other agents known to affect cardiac contractility and/or conduction.
Pregnancy and Lactation
Diltiazem hydrochloride is teratogenic in some animal species. In the absence of adequate evidence of safety in human pregnancy, ALTIAZEM should not be used in pregnancy or in women of child-bearing potential. If it is considered essential that diltiazem hydrochloride be given to a woman of child-bearing potential, the possibility of pregnancy must be excluded before starting the treatment and adequate contraception must be used throughout the therapy.
Diltiazem hydrochloride is excreted in breast milk. If use of ALTIAZEM is considered essential, another method of infant feeding should be instituted.
Effects on ability to drive and to use machines
No studies on ability to drive or use machines have been performed.
Side effects such as dizziness or syncope can occur, particularly at start of treatment or after changes in dose and patients should ensure they do not have these effects before driving or operating machinery.
Undesirable Effects
Immune system disorders: More rarely, cases of angioneurotic oedema have been reported.
Psychiatric disorders: Nervousness, insomnia.
Cardiac disorders: Rare cases of symptomatic bradycardia, sinoatrial block and atrioventricular block, palpitations have been reported. Development or aggravation of congestive heart failure.
Vascular disorders: Effects of vasodilation may include orthostatic hypotension, headache, flushing and particularly lower limb oedema. These effects are related to pharmacologic activity and are dose dependent, and may be more frequent in the elderly. Occasional reports of vasculitis, including leukocytoclastic vasculitis.
Gastrointestinal disorders: Abdominal pain, nausea, constipation, dry mouth, dyspepsia, diarrhoea, vomiting, gingival hyperplasia.
Hepatobiliary disorders: Rare cases of increase of hepatic transaminase have been also reported. However such increases are rare, moderate and transient, and occur at start of therapy. Very rare and exceptional cases of clinical hepatitis have been also reported which resolved on cessation of diltiazem therapy.
Skin and Subcutaneous tissue disorders: Erythema, urticarial reactions, desquamative erythema, with or without fever and photosensitivity which resolve when treatment is discontinued. More rarely Erythema multiforme (including rare cases of Stevens-Johnson's syndrome) and/or exfoliative dermatitis, and acute generalised exanthematous pustular dermatitis have been reported. Very rare cases of toxic Epidermal Necrolysis have also been reported.
Other: Malaise, dizziness, asthenia, fatigue. Very rare cases of gynaecomastia and extrapyramidal symptoms have been reported which are reversible upon discontinuation.
Overdose
Experience of overdosage in man is limited, but cases of spontaneous recovery have been reported. However, it is recommended that patients with suspected overdose should be placed under observation in a coronary care unit with facilities available for treatment of any possible hypotension and conduction disturbances that may occur.
Most patients suffering from overdosage of diltiazem become hypotensive within 8 hours of ingestion. With bradycardia and first to third degree atrioventricular block also developing, cardiac arrest may ensue. Hyperglycaemia is also a recognised complication. The elimination half-life of diltiazem after overdosage is estimated to be about 5.5-10.2 hours.
If a patient presents early after overdose, gastric lavage should be performed and activated charcoal administered to reduce diltiazem absorption.
Hypotension should be corrected with plasma expanders, intravenous calcium gluconate and inotropic agents (dopamine, dobutamine or isoprenaline).
Symptomatic bradycardia and high grade AV block may respond to atropine, isoprenaline or occasionally cardiac pacing which may be useful if cardiac standstill occurs.
ALTIAZEM Tablets are sustained release tablets and effects may be slow in onset and prolonged, therefore, monitoring should be carried out for longer periods than following overdose with immediate release dosage forms.
Pharmacodynamic properties:
Pharmacotherapeutic group: Calcium channel blocker.
Diltiazem is a benzothiazepine calcium-channel blocking agent. These agents interfere with the influx of calcium ions through the slow channels of active cell membranes, influencing the myocardial cells, the cells within the specialised conducting system of the heart and the cells of vascular smooth muscle.
It is used in the management of classical and vasospastic angina pectoris. The efficacy of diltiazem in the treatment of angina pectoris is probably related to its coronary vasodilating properties (causing an increase in myocardial oxygen supply) and to some of its haemodynamic effects (resulting in a decrease in myocardial work/oxygen demand).
Although diltiazem is a potent vasodilator, the reduction in blood pressure that often accompanies its use usually occurs without reflex tachycardia, as diltiazem has little effect on the peripheral vasculature.
Diltiazem causes a small reduction in heart rate which is accompanied by an increase in cardiac output, improved myocardial perfusion and reduction of ventricular work.
Diltiazem has a less negative inotropic effect than verapamil and significant myocardial depression rarely occurs.
Pharmacokinetic properties:
Diltiazem hydrochloride is effective in angina, protecting the heart against ischaemia, vasodilating coronary arteries and reducing myocardial oxygen requirements. It is well tolerated and does not generally give rise to side effects associated with peripheral vasodilators, nor cause significant myocardial depression.
Diltiazem is rapidly and almost completely (about 90%) absorbed from the gastrointestinal tract after oral administration. However, it is subject to extensive first-pass hepatic metabolism, reported to reduce the bioavailability to about 40%. The absolute bioavailability is dose related.
Peak plasma concentration is reached within about 3-4 hours after oral dosing and steady-state plasma concentrations are reached in about 3 days.
The mean volume of distribution is about 5L/kg. Diltiazem is highly lipophilic and appears in cerebrospinal fluid (rabbit studies) and in breast milk. It is highly protein bound (80-90%), as is its most active metabolite, desacetyl diltiazem (60-75%).
Diltiazem is extensively metabolised, the most important metabolites being N-mono-desmethyl diltiazem (with 20% of potency of diltiazem), desacetyl diltiazem (50% relative potency) and N-demethyl desacetyl diltiazem. The metabolites are detectable in plasma within 30 minutes, reaching concentrations of 30-50%, 10-30% and 10-20% of the parent drug, respectively.
The elimination half-life of oral diltiazem is about 4-8 hours and it is longer for the metabolites. Excretion of diltiazem and its metabolites is mainly in the urine. Less than 4% of a dose of diltiazem is excreted in the urine as unchanged drug within 24 hours.
There is a linear relationship between dose and plasma concentration. During long-term administration to any one patient, plasma concentrations of diltiazem remain constant.
Mean plasma concentrations in elderly subjects and patients with renal and hepatic insufficiency are higher than in young subjects.
Diltiazem and its metabolites are poorly dialyzed.
Storage
Store at temperature not exceeding 30°C.
Store in the original package.
Keep container in the outer carton.
Packaging
ALTIAZEM 60 mg MR Tablets: Box containing 2 blisters of 10 MR tablets each.
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: