- Anti-hestaminic & Respiratory Drugs (20)
- Anti-inflammatory Drugs (197) +-
- Baby & Mom (1346) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (52)
- Beauty (3129) +-
- Beauty > Skin Care > whitening (309)
- Chemotherapy & Immune Response (885) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (11)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (290)
- CIRCULATORY DISTURBANCE AGENTS (24)
- Diet & Fitness Products (284) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (191)
- HEMATOLOGY (39)
-
Medical Supplies (506)
+-
- Chemicals & Disinfectants (19)
- Dental Supplies (31)
- Devices & Instruments (11)
- Diabetic Supplies (121)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- KIDNEY UNIT SUPPLIES (21)
- Lab Supplies (3)
- Miscellaneous (21)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (2)
- Sanitary (5)
- Sterilization Supplies (1)
- Surgical Sutures (4)
- Syringes (3)
-
Medicines & Health (2727)
+-
- Allergy & Sinus (97)
- Children's Health Care (54)
- Cough, Cold & Flu (283)
- Digestive Health & Nausea (231)
- Ear, Nose & Throat Care (181)
- Eye Care (124)
- Feminine Care (323)
- Foot Care (12)
- Orthopaedic Appliances (1)
- Pain Relief & Management (244)
- Pill Organizer (2)
- Skin Treatments (863)
- Sleep & Snoring Aids (2)
- Support & Braces (8)
- Medicines & health > Gout releif (42)
- Natural & Organic Products (81) +-
- OTC > Analgesics > Anti-inflammatory Drugs (44)
-
Personal Care (3363)
+-
- Bath & Body (273)
- Deodorant & Anti-perspirants (191)
- Ear, Nose & Throat Care (177)
- Eye Care (131)
- Feminine Care (372)
- Foot Care (20)
- Hair Care (511)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (26)
- Massage & Relaxation (17)
- Natural & Organic Personal Care (7)
- Oral Care (91)
- Pregnancy & Fertility (64)
- Shaving & Grooming (75)
- Sun Care (80)
-
Prescription Drugs (2935)
+-
- Analgesics (184)
- Cardiovascular System (377)
- Drugs Affecting Musculoskeletal System (65)
- Drugs Used In Infections (56)
- Ear & Nose Drugs (2)
- Endocrine System (177)
- Gastrointestinal Tract (243)
- Gastrointestinal Tract > Hepatology > Liver treatment (60)
- GYNECOLOGY (2)
- Miscellaneous (11)
- NEPHROLOGY > URINARY SYSTEM > RENAL DISORDERS > URINARY TRACT DISORDERS (47)
- NEUROLOGY (228)
- Nutrients & Blood Electrolytes (2)
- Respiratory System (154)
- SKIN > NAILS > HAIR > TOPICAL PREPARATIONS (115)
- Vaccines (1)
- Prescription drugs > Cardiovascular system > Anti-hypertension drugs (242)
- Sexual Wellness (304) +-
- Vitamins & Minerals Supplements (1230) +-
Ex Tax: 78EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.
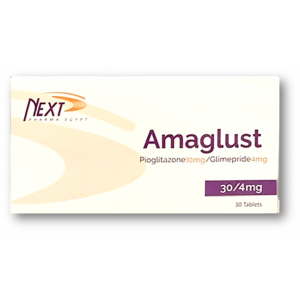
INDICATIONS
AMARYL is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus [see Clinical Studies].
Important Limitations Of Use
AMARYL should not be used for the treatment of type 1 diabetes mellitus or diabetic ketoacidosis, as it would not be effective in these settings.
DOSAGE AND ADMINISTRATION
Recommended Dosing
AMARYL should be administered with breakfast or the first main meal of the day.
The recommended starting dose of AMARYL is 1 mg or 2 mg once daily. Patients at increased risk for hypoglycemia (e.g., the elderly or patients with renal impairment) should be started on 1 mg once daily [see WARNINGS AND PRECAUTIONS and Use in Specific Populations].
After reaching a daily dose of 2 mg, further dose increases can be made in increments of 1 mg or 2 mg based upon the patient's glycemic response. Uptitration should not occur more frequently than every 1-2 weeks. A conservative titration scheme is recommended for patients at increased risk for hypoglycemia [see WARNINGS AND PRECAUTIONS and Use in Specific Populations].
The maximum recommended dose is 8 mg once daily.
Patients being transferred to AMARYL from longer half-life sulfonylureas (e.g., chlorpropamide) may have overlapping drug effect for 1-2 weeks and should be appropriately monitored for hypoglycemia.
When colesevelam is coadministered with glimepiride, maximum plasma concentration and total exposure to glimepiride is reduced. Therefore, AMARYL should be administered at least 4 hours prior to colesevelam.
HOW SUPPLIED
Dosage Forms And Strengths
AMARYL is formulated as tablets of:
- 1 mg (pink, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side)
- 2 mg (green, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side)
- 4 mg (blue, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side)
Storage And Handling
AMARYL tablets are available in the following strengths and package sizes:
1 mg (pink, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side) in bottles of 100 (NDC 0039-0221-10)
2 mg (green, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side) in bottles of 100 (NDC 0039-0222-10)
4 mg (blue, flat-faced, oblong with notched sides at double bisect, imprinted with “AMA RYL” on one side) in bottles of 100 (NDC 0039-0223-10)
Store at 25°C (77°F); excursions permitted to 20 - 25°C (68 - 77°F) (see USP Controlled Room Temperature).
Dispense in well-closed containers with safety closures.
sanofi-aventis U.S. LLC, Bridgewater, NJ 08807, A SANOFI COMPANY. Revised Dec 2016
SIDE EFFECTS
The following serious adverse reactions are discussed in more detail below and elsewhere in the labeling:
- Hypoglycemia [see WARNINGS AND PRECAUTIONS]
- Hemolytic anemia [see WARNINGS AND PRECAUTIONS]
In clinical trials, the most common adverse reactions with AMARYL were hypoglycemia, dizziness, asthenia, headache, and nausea.
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Approximately 2,800 patients with type 2 diabetes have been treated with AMARYL in the controlled clinical trials. In these trials, approximately 1,700 patients were treated with AMARYL for at least 1 year.
Table 1 summarizes adverse events, other than hypoglycemia, that were reported in 11 pooled placebocontrolled trials, whether or not considered to be possibly or probably related to study medication. Treatment duration ranged from 13 weeks to 12 months. Terms that are reported represent those that occurred at an incidence of ≥ 5% among AMARYL-treated patients and more commonly than in patients who received placebo.
Table 1: Eleven Pooled Placebo-Controlled Trials ranging from 13 weeks to 12 months : Adverse Events (Excluding Hypoglycemia) Occurring in ≥ 5% of AMARYL-treated Patients and at a Greater Incidence than with Placebo*
| AMARYL N=745 % |
Placebo N=294 % |
|
| Headache | 8.2 | 7.8 |
| Accidental Injury† | 5.8 | 3.4 |
| Flu Syndrome | 5.4 | 4.4 |
| Nausea | 5.0 | 3.4 |
| Dizziness | 5.0 | 2.4 |
| *AMARYL doses ranged from 1-16 mg administered daily †Insufficient information to determine whether any of the accidental injury events were associated with hypoglycemia |
||
Hypoglycemia
In a randomized, double-blind, placebo-controlled monotherapy trial of 14 weeks duration, patients already on sulfonylurea therapy underwent a 3-week washout period then were randomized to AMARYL 1 mg, 4 mg, 8 mg or placebo. Patients randomized to AMARYL 4 mg or 8 mg underwent forced-titration from an initial dose of 1 mg to these final doses, as tolerated [see Clinical Studies]. The overall incidence of possible hypoglycemia (defined by the presence of at least one symptom that the investigator believed might be related to hypoglycemia; a concurrent glucose measurement was not required) was 4% for AMARYL 1 mg, 17% for AMARYL 4 mg, 16% for AMARYL 8 mg and 0% for placebo. All of these events were self-treated.
In a randomized, double-blind, placebo-controlled monotherapy trial of 22 weeks duration, patients received a starting dose of either 1 mg AMARYL or placebo daily. The dose of AMARYL was titrated to a target fasting plasma glucose of 90-150 mg/dL. Final daily doses of AMARYL were 1, 2, 3, 4, 6 or 8 mg [see Clinical Studies]. The overall incidence of possible hypoglycemia (as defined above for the 14-week trial) for AMARYL vs. placebo was 19.7% vs. 3.2%. All of these events were selftreated.
Weight gain: AMARYL, like all sulfonylureas, can cause weight gain [see Clinical Studies].
Allergic Reactions: In clinical trials, allergic reactions, such as pruritus, erythema, urticaria, and morbilliform or maculopapular eruptions, occurred in less than 1% of AMARYL-treated patients. These may resolve despite continued treatment with AMARYL. There are postmarketing reports of more serious allergic reactions (e.g., dyspnea, hypotension, shock) [see WARNINGS AND PRECAUTIONS].
Laboratory Tests
Elevated Serum Alanine Aminotransferase (ALT): In 11 pooled placebo-controlled trials of AMARYL, 1.9% of AMARYL-treated patients and 0.8% of placebo-treated patients developed serum ALT greater than 2 times the upper limit of the reference range.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of AMARYL. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Serious hypersensitivity reactions, including anaphylaxis, angioedema, and Stevens-Johnson Syndrome [see WARNINGS AND PRECAUTIONS]
- Hemolytic anemia in patients with and without G6PD deficiency [see WARNINGS AND PRECAUTIONS]
- Impairment of liver function (e.g. with cholestasis and jaundice), as well as hepatitis, which may progress to liver failure.
- Porphyria cutanea tarda, photosensitivity reactions and allergic vasculitis
- Leukopenia, agranulocytosis, aplastic anemia, and pancytopenia
- Thrombocytopenia (including severe cases with platelet count less than 10,000/μL) and thrombocytopenic purpura
- Hepatic porphyria reactions and disulfiram-like reactions
- Hyponatremia and syndrome of inappropriate antidiuretic hormone secretion (SIADH), most often in patients who are on other medications or who have medical conditions known to cause hyponatremia or increase release of antidiuretic hormone
- Dysgeusia
- Alopecia
DRUG INTERACTIONS
Drugs Affecting Glucose Metabolism
A number of medications affect glucose metabolism and may require AMARYL dose adjustment and particularly close monitoring for hypoglycemia or worsening glycemic control.
The following are examples of medications that may increase the glucose-lowering effect of sulfonylureas including AMARYL, increasing the susceptibility to and/or intensity of hypoglycemia: oral anti-diabetic medications, pramlintide acetate, insulin, angiotensin converting enzyme (ACE) inhibitors, H2 receptor antagonists, fibrates, propoxyphene, pentoxifylline, somatostatin analogs, anabolic steroids and androgens, cyclophosphamide, phenyramidol, guanethidine, fluconazole, sulfinpyrazone, tetracyclines, clarithromycin, disopyramide, quinolones, and those drugs that are highly protein-bound, such as fluoxetine, nonsteroidal anti-inflammatory drugs, salicylates, sulfonamides, chloramphenicol, coumarins, probenecid and monoamine oxidase inhibitors. When these medications are administered to a patient receiving AMARYL, monitor the patient closely for hypoglycemia. When these medications are withdrawn from a patient receiving AMARYL, monitor the patient closely for worsening glycemic control.
The following are examples of medications that may reduce the glucose-lowering effect of sulfonylureas including AMARYL, leading to worsening glycemic control: danazol, glucagon, somatropin, protease inhibitors, atypical antipsychotic medications (e.g., olanzapine and clozapine), barbiturates, diazoxide, laxatives, rifampin, thiazides and other diuretics, corticosteroids, phenothiazines, thyroid hormones, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics (e.g., epinephrine, albuterol, terbutaline), and isoniazid. When these medications are administered to a patient receiving AMARYL, monitor the patient closely for worsening glycemic control. When these medications are withdrawn from a patient receiving AMARYL, monitor the patient closely for hypoglycemia.
Beta-blockers, clonidine, and reserpine may lead to either potentiation or weakening of AMARYL's glucose-lowering effect.
Both acute and chronic alcohol intake may potentiate or weaken the glucose-lowering action of AMARYL in an unpredictable fashion.
The signs of hypoglycemia may be reduced or absent in patients taking sympatholytic drugs such as beta-blockers, clonidine, guanethidine, and reserpine.
Miconazole
A potential interaction between oral miconazole and sulfonylureas leading to severe hypoglycemia has been reported. Whether this interaction also occurs with other dosage forms of miconazole is not known.
Cytochrome P450 2C9 Interactions
There may be an interaction between glimepiride and inhibitors (e.g., fluconazole) and inducers (e.g., rifampin) of cytochrome P450 2C9. Fluconazole may inhibit the metabolism of glimepiride, causing increased plasma concentrations of glimepiride which may lead to hypoglycemia. Rifampin may induce the metabolism of glimepiride, causing decreased plasma concentrations of glimepiride which may lead to worsening glycemic control.
Concomitant Administration Of Colesevelam
Colesevelam can reduce the maximum plasma concentration and total exposure of glimepiride when the two are coadministered. However, absorption is not reduced when glimepiride is administered 4 hours prior to colesevelam. Therefore, AMARYL should be administered at least 4 hours prior to colesevelam.
WARNINGS
Included as part of the PRECAUTIONS section.
PRECAUTIONS
Hypoglycemia
All sulfonylureas, including AMARYL, can cause severe hypoglycemia [see ADVERSE REACTIONS]. The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. These impairments may present a risk in situations where these abilities are especially important, such as driving or operating other machinery. Severe hypoglycemia can lead to unconsciousness or convulsions and may result in temporary or permanent impairment of brain function or death.
Patients must be educated to recognize and manage hypoglycemia. Use caution when initiating and increasing AMARYL doses in patients who may be predisposed to hypoglycemia (e.g., the elderly, patients with renal impairment, patients on other anti-diabetic medications). Debilitated or malnourished patients, and those with adrenal, pituitary, or hepatic impairment are particularly susceptible to the hypoglycemic action of glucose-lowering medications. Hypoglycemia is also more likely to occur when caloric intake is deficient, after severe or prolonged exercise, or when alcohol is ingested.
Early warning symptoms of hypoglycemia may be different or less pronounced in patients with autonomic neuropathy, the elderly, and in patients who are taking beta-adrenergic blocking medications or other sympatholytic agents. These situations may result in severe hypoglycemia before the patient is aware of the hypoglycemia.
Hypersensitivity Reactions
There have been postmarketing reports of hypersensitivity reactions in patients treated with AMARYL, including serious reactions such as anaphylaxis, angioedema, and Stevens-Johnson Syndrome. If a hypersensitivity reaction is suspected, promptly discontinue AMARYL, assess for other potential causes for the reaction, and institute alternative treatment for diabetes.
Hemolytic Anemia
Sulfonylureas can cause hemolytic anemia in patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency. Because AMARYL is a sulfonylurea, use caution in patients with G6PD deficiency and consider the use of a non-sulfonylurea alternative. There are also postmarketing reports of hemolytic anemia in patients receiving AMARYL who did not have known G6PD deficiency [see ADVERSE REACTIONS].
Increased Risk Of Cardiovascular Mortality With Sulfonylureas
The administration of oral hypoglycemic drugs has been reported to be associated with increased cardiovascular mortality as compared to treatment with diet alone or diet plus insulin. This warning is based on the study conducted by the University Group Diabetes Program (UGDP), a long-term, prospective clinical trial designed to evaluate the effectiveness of glucose-lowering drugs in preventing or delaying vascular complications in patients with non-insulin-dependent diabetes. The study involved 823 patients who were randomly assigned to one of four treatment groups UGDP reported that patients treated for 5 to 8 years with diet plus a fixed dose of tolbutamide (1.5 grams per day) had a rate of cardiovascular mortality approximately 2-½ times that of patients treated with diet alone. A significant increase in total mortality was not observed, but the use of tolbutamide was discontinued based on the increase in cardiovascular mortality, thus limiting the opportunity for the study to show an increase in overall mortality. Despite controversy regarding the interpretation of these results, the findings of the UGDP study provide an adequate basis for this warning. The patient should be informed of the potential risks and advantages of AMARYL and of alternative modes of therapy. Although only one drug in the sulfonylurea class (tolbutamide) was included in this study, it is prudent from a safety standpoint to consider that this warning may also apply to other oral hypoglycemic drugs in this class, in view of their close similarities in mode of action and chemical structure.
Macrovascular Outcomes
There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with AMARYL or any other anti-diabetic drug.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, And Impairment Of Fertility
Studies in rats at doses of up to 5000 parts per million (ppm) in complete feed (approximately 340 times the maximum recommended human dose, based on surface area) for 30 months showed no evidence of carcinogenesis. In mice, administration of glimepiride for 24 months resulted in an increase in benign pancreatic adenoma formation that was dose-related and was thought to be the result of chronic pancreatic stimulation. No adenoma formation in mice was observed at a dose of 320 ppm in complete feed, or 46-54 mg/kg body weight/day. This is about 35 times the maximum human recommended dose of 8 mg once daily based on surface area.
Glimepiride was non-mutagenic in a battery of in vitro and in vivo mutagenicity studies (Ames test, somatic cell mutation, chromosomal aberration, unscheduled DNA synthesis, and mouse micronucleus test).
There was no effect of glimepiride on male mouse fertility in animals exposed up to 2500 mg/kg body weight ( > 1,700 times the maximum recommended human dose based on surface area). Glimepiride had no effect on the fertility of male and female rats administered up to 4000 mg/kg body weight (approximately 4,000 times the maximum recommended human dose based on surface area).
Use In Specific Populations
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of AMARYL in pregnant women. In animal studies there was no increase in congenital anomalies, but an increase in fetal deaths occurred in rats and rabbits at glimepiride doses 50 times (rats) and 0.1 times (rabbits) the maximum recommended human dose (based on body surface area). This fetotoxicity, observed only at doses inducing maternal hypoglycemia, is believed to be directly related to the pharmacologic (hypoglycemic) action of glimepiride and has been similarly noted with other sulfonylureas. AMARYL should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Because data suggest that abnormal blood glucose during pregnancy is associated with a higher incidence of congenital abnormalities, diabetes treatment during pregnancy should maintain blood glucose as close to normal as possible.
Nonteratogenic Effects
Prolonged severe hypoglycemia (4 to 10 days) has been reported in neonates born to mothers receiving a sulfonylurea at the time of delivery.
Nursing Mothers
It is not known whether AMARYL is excreted in human milk. During pre- and post-natal studies in rats, significant concentrations of glimepiride were present in breast milk and the serum of the pups. Offspring of rats exposed to high levels of glimepiride during pregnancy and lactation developed skeletal deformities consisting of shortening, thickening, and bending of the humerus during the postnatal period. These skeletal deformations were determined to be the result of nursing from mothers exposed to glimepiride. Based on these animal data and the potential for hypoglycemia in a nursing infant, a decision should be made whether to discontinue nursing or discontinue AMARYL, taking into account the importance of AMARYL to the mother.
Pediatric Use
The pharmacokinetics, efficacy and safety of AMARYL have been evaluated in pediatric patients with type 2 diabetes as described below. AMARYL is not recommended in pediatric patients because of its adverse effects on body weight and hypoglycemia.
The pharmacokinetics of a 1 mg single dose of AMARYL was evaluated in 30 patients with type 2 diabetes (male = 7; female = 23) between ages 10 and 17 years. The mean (± SD) AUC (339±203 ng·hr/mL), Cmax (102±48 ng/mL) and t½ (3.1±1.7 hours) for glimepiride were comparable to historical data from adults (AUC(0-last) 315±96 ng·hr/mL, Cmax 103±34 ng/mL and t½ 5.3±4.1 hours).
The safety and efficacy of AMARYL in pediatric patients was evaluated in a single-blind, 24-week trial that randomized 272 patients (8-17 years of age) with type 2 diabetes to AMARYL (n=135) or metformin (n=137). Both treatment-naive patients (those treated with only diet and exercise for at least 2 weeks prior to randomization) and previously treated patients (those previously treated or currently treated with other oral antidiabetic medications for at least 3 months) were eligible to participate. Patients who were receiving oral antidiabetic agents at the time of study entry discontinued these medications before randomization without a washout period. AMARYL was initiated at 1 mg, and then titrated up to 2, 4 or 8 mg (mean last dose 4 mg) through Week 12, targeting a self-monitored fasting fingerstick blood glucose < 126 mg/dL. Metformin was initiated at 500 mg twice daily and titrated at Week 12 up to 1000 mg twice daily (mean last dose 1365 mg).
After 24 weeks, the overall mean treatment difference in HbA1c between AMARYL and metformin was 0.2%, favoring metformin (95% confidence interval -0.3% to +0.6%). Based on these results, the trial did not meet its primary objective of showing a similar reduction in HbA1c with AMARYL compared to metformin.
Table 2: Change from Baseline in HbA and Body Weight in Pediatric Patients Taking Amaryl or Metformin
| Metformin | AMARYL | |
| Treatment-Naive Patients* | N=69 | N=72 |
| HbA1C (%) | ||
| Baseline (mean) | 8.2 | 8.3 |
| Change from baseline (adjusted LS mean)† | -1.2 | -1.0 |
| Adjusted Treatment Difference‡(95%CI) | 0.2 (-0.3; 0.6) | |
| Previously Treated Patients* | N=57 | N=55 |
| HbA1C (%) | ||
| Baseline (mean) | 9.0 | 8.7 |
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: