- Anti-hestaminic & Respiratory Drugs (14)
- Anti-inflammatory Drugs (130)
- Baby & Mom (1115) +-
- Baby & Mom > Bath, skin & Hair > Skin Care > wibes (47)
- Beauty (2387) +-
- Beauty > Skin Care > whitening (230)
- Chemotherapy & Immune Response (253) +-
- Chemotherapy & Immune Response > ANTI-FUNGAL (2)
- Chemotherapy & Immune Response > Chemotherapeutic Agents > Hormone Antagonists >Enzyme Inhibitors (82)
- CIRCULATORY DISTURBANCE AGENTS (15)
- CORTECOSTEROIDS (3)
- Diet & Fitness Products (186) +-
- DRUG AFFECTING CENTRAL NERVOUS SYSTEM (138)
- Drugs affecting CNS >Anti- epileptic (46)
- LIVER SUPPORT>MULTIVITAMINS (22)
-
Medical Supplies (445)
+-
- Chemicals & Disinfectants (18)
- Dental Supplies (31)
- Devices & Instruments (7)
- Diabetic Supplies (91)
- General Medical Supplies (21)
- I.V & Medical Solution (0)
- Intensive Care Unit & Anesthesia Supplies (0)
- Kindney Unit Supplies (13)
- Lab Supplies (1)
- Miscellaneous (22)
- Neonatal Unit Supplies (0)
- Operation Room Supplies (4)
- Sanitary (5)
- Sterilization Supplies (0)
- Surgical Sutures (4)
- Syringes (2)
-
Medicines & Health (2163)
+-
- Allergy & Sinus (84)
- Children's Health Care (46)
- Cough, Cold & Flu (257)
- Digestive Health & Nausea (178)
- Ear, Nose & Throat Care (148)
- Eye Care (102)
- Feminine Care (283)
- Foot Care (3)
- Orthopaedic Appliances (0)
- Pain Relief & Management (180)
- Pill Organizer (0)
- Skin Treatments (633)
- Sleep & Snoring Aids (0)
- Support & Braces (7)
- Medicines & health > Gout releif (34)
- Natural & Organic Products (58) +-
- OTC > Analgesics > Anti-inflammatory Drugs (32)
-
Personal Care (2686)
+-
- Bath & Body (214)
- Deodorant & Anti-perspirants (159)
- Ear, Nose & Throat Care (141)
- Eye Care (108)
- Feminine Care (317)
- Foot Care (10)
- Hair Care (346)
- Home Tests & Monitorings (14)
- Incontinence (7)
- Lip Care (19)
- Massage & Relaxation (14)
- Natural & Organic Personal Care (6)
- Oral Care (76)
- Pregnancy & Fertility (51)
- Shaving & Grooming (55)
- Sun Care (52)
- Prescribtion drugs > cardiovascular system > Hypertention drugs (201)
-
Prescription Drugs (2143)
+-
- Analgesics (149)
- Cardiovascular System (269)
- Drugs Affecting CNS (155)
- Drugs Affecting Musculoskeletal System (46)
- Drugs Used In Infections (28)
- Ear & Nose Drugs (2)
- Endocrine System (124)
- Gastrointestinal Tract (178)
- Gastrointestinal Tract (165)
- Miscellaneous (2)
- Nutrients & Blood Electrolytes (0)
- Obstetric & Gynaecology Disorders (1)
- Respiratory System (96)
- Topical Preparations (21)
- Urinary Tract Disorders (12)
- Vaccines (0)
- Prescription Drugs > Cardiovascular System > Anti-hypertensive drugs > Duiretics > Loop duiretics (41)
- prescription drugs > cardiovascular system >Anti-hypertensive drugs > duiretics > Aldosterone antagonist duiretics (62)
- prescription drugs > cardiovascular system >Anti-hypertensive drugs > duiretics > duiretic combinations (59)
- prescription drugs > cardiovascular system >Anti-hypertensive drugs > duiretics > loop duiretics (59)
- Prescription Drugs > Gastrointestinal Tract > Liver treatment (46)
- Sexual Wellness (163) +-
- strong anti-emetic & adjuvent used with anti-neoplastic (1)
- Vitamins & Minerals Supplements (392)
- Vitamins & Supplements> folic acid (1597) +-
Availability: In Stock
Ex Tax: 5,277EGP
Example
You can return the product within 14 days of purchase.
ReturnsYou can return the product within 14 days of purchase.

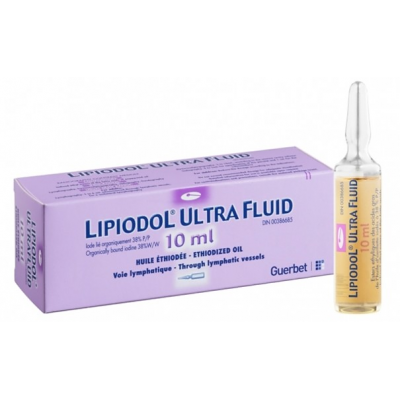
Lipiodol Ultra-Fluide Injection
Ethiodized oil
( 480 mg / mL Iodine organically + ethyl esters of fatty acids of poppy seed oil ) 10 mL ampoule
Warning
Injection route (Oil)
Inadvertent intravascular injection or intravasation of ethiodized oil may cause pulmonary and cerebral embolism. Inject slowly with radiologic monitoring; do not exceed recommended dose.
Along with its needed effects, ethiodized oil (the active ingredient contained in Lipiodol Ultra-Fluide) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor or nurse immediately if any of the following side effects occur while taking ethiodized oil:
Incidence Not Known
- Abdominal or stomach pain
- anxiety
- bloated abdomen or stomach
- changes in vision
- chest pain or tightness
- cough
- decreased frequency or amount of urine
- depressed mood
- difficulty with swallowing
- dizziness or lightheadedness
- fainting
- fast heartbeat
- fever
- headache
- inflamed tissue from infection
- loss of appetite
- lower back or side pain
- muscle cramps and stiffness
- nausea or vomiting
- pain and fullness in the right upper abdomen or stomach
- pain, tenderness, or swelling of the foot or leg
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- skin rash, hives, itching, or redness
- sudden shortness of breath or troubled breathing
- sweating
- swelling of the face, fingers, or lower legs
- trouble sleeping
- unusual tiredness or weakness
- weight gain or loss
- yellow eyes and skin
-
Some side effects of ethiodized oil may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence Not Known
- Delayed healing at the incision site
- diarrhea
1. NAME OF THE MEDICINAL PRODUCT
LIPIODOL ULTRA-FLUID (480 mg I/ml), solution for injection.
4.1. Therapeutic indications4.2. Posology and route of administration
- Lymphography
- Diagnosis of hepatic lesions
Patients with low weight
The dose must be reduced proportionally in this population.
Elderly
The product must be administered with special care in patients over 65 years of age with underlying diseases of the cardiovascular, respiratory or nervous systems. Keeping in mind that part of the product temporarily embolises the pulmonary capillaries, the dose must be adjusted in elderly patients with cardiorespiratory failure or the examination must be cancelled.
In interventional radiology
The administration is by selective intra-arterial catheterism of the hepatic artery. The procedure should be performed within a typical interventional radiology setting with the appropriate equipment. The dose of LIPIODOL ULTRA-FLUID depends on the extent of the lesion, but should usually not exceed a total dose of 15 mL in adults.
LIPIODOL ULTRA-FLUID can be mixed with anticancer drugs such as cisplatin, doxorubicin, epirubicin and mitomycin. Instructions and precautions for use of the anticancer drugs must be strictly followed.
Instructions for preparation of the mixture of LIPIODOL ULTRA-FLUID with an anticancer drug:
The procedure can be repeated every 4 to 8 weeks according to tumour response and patient conditions.
Paediatric population
The efficacy and safety of the use of LIPIODOL ULTRA-FLUID for Trans-Arterial Chemo-Embolisation of hepatocellular carcinoma have not been established in children.
Elderly
The product must be administered with special care in patients over 65 years of age with underlying diseases of the cardiovascular, respiratory or nervous systems.
Exclusive selective arterial catheterization.
The dose of LIPIODOL ULTRA-FLUID per embolisation session is determined depending on the size of the lesions. The proportion of LIPIODOL ULTRA-FLUID versus the liquid embolising agent can vary from 20 to 80% but is usually a 50/50 mixture.
The injection volume must not exceed 15 mL.
In endocrinology:
Strict intramuscular route.
In patients with thyroid nodules, the dose is 0.2 mL.
4.3. Contraindications
- Trans-Arterial Chemo-Embolisation of hepatocellular carcinoma:
- Prepare two syringes large enough to contain the total volume of mixture. The first syringe contains the anticancer drug solution, the second syringe contains LIPIODOL ULTRA-FLUID.
- Connect the two syringes to a 3-way stopcock.
- Perform 15 to 20 back and forth movements between the two syringes to obtain a homogeneous mixture. It is recommended to start by pushing the syringe with the anticancer drug first.
- The mixture is to be prepared at the time of use and must be used promptly after preparation (within 3 hours). If necessary during the interventional radiology procedure, the mixture can be re-homogenised as described above.
- When the adequate mixture is obtained, use a 1 to 3 mL syringe to inject in the micro-catheter.
- Embolisation with surgical glues
- Adults and children over 4 years of age: 1 mL every three years.
- Children under 4 years of age : 0.5 mL every two years without exceeding 3 mL.
- Hypersensitivity to LIPIODOL ULTRA-FLUID (ethyl esters of iodised fatty acids of poppyseed oil).
- Pregnant women
- Confirmed hyperthyroidism.
- Traumatic lesions, haemorrhage or recent bleeding (risk of extravasation or embolism).
- Bronchography (the product rapidly inundates the bronchioles and alveoli).
Contraindications specific to the use in interventional radiology:
Administration in liver areas with dilated bile ducts unless drainage has been performed.
There are no particular contraindications apart from those of embolization, particularly in patients with portal vein thrombosis.
Contraindications specific to the use in endocrinology:
4.4. Special warnings and special precautions for use
- Trans-Arterial Chemo-Embolisation
- Embolisation with surgical glues
- Large multinodular goiter in patients over 45 years of age, because of the high risk of hyperthyroidism,
- During breastfeeding.
-
Hepatic intra-arterial procedures can cause an irreversible liver insufficiency in patients with serious liver malfunction and/or undergoing close multiple sessions. More than 50% liver replacement with tumour, bilirubin level greater than 2 mg/dL, lactate dehydrogenase level greater than 425 mg/dL, aspartate aminotransferase level greater than 100 IU/L and decompensated cirrhosis have been described as associated with increased post-procedural mortality.
Oesophageal varices must be carefully monitored as they can rupture immediately after treatment. If a risk of rupture is demonstrated, endoscope sclerotherapy/ligature should be performed before the Trans-Arterial Chemo-Embolisation procedure.
Iodinated contrast agent induced renal insufficiency must be systematically prevented by correct rehydration before and after The procedure.
The risk of superinfection in the treated area is normally prevented by administration of antibiotics.
4.4.1.5. Embolisation with surgical glues
An early polymerisation reaction may exceptionally occur between LIPIODOL ULTRA-FLUID and certain surgical glues, or even certain batches of glue. Before using new batches of LIPIODOL ULTRA-FLUID or surgical glue, the compatibility of LIPIODOL ULTRA-FLUID and the glue must be tested in vitro.
4.4.2 Precautions for use
4.4.2.1. Hypersensitivity
Before the examination:
identify patients at risk in a detailed interview on their history.
Corticosteroids and H1 antihistamines have been proposed as premedication in patients at greatest risk for hypersensitivity reactions (patients with known hypersensitivity to a contrast agent). However, they do not prevent the occurrence of serious or fatal anaphylactic shock.
Throughout the examination, maintain:
After the examination:
After contrast agent administration, the patient must be monitored for at least 30 minutes, as most serious adverse reactions occur within this time period.
The patient must be warned of the possibility of delayed reactions (for up to seven days) (see Section 4.8 - Undesirable effects).
4.4.2.2. Thyroid
Possible thyroid risk factors must be investigated to prevent metabolic disorders. If iodinated contrast agents are to be administered to patients at risk, thyroid function tests must be carried out before the examination.
4.4.2.3. Trans-Arterial Chemo-Embolisation / Embolisation
Iodinated contrast agents can induce a transient deterioration of renal function or exacerbate pre-existing renal failure. The preventive measures are as follows:
- medical monitoring
- an indwelling intravenous catheter.
- Identify patients at risk, i.e. patients who are dehydrated or who have renal failure, diabetes, severe heart failure, monoclonal gammopathy (multiple myeloma, Waldenstrom's macroglobulinemia), a history of renal failure after administration of iodinated contrast agents, children under one year of age and elderly atheromatous subjects.
- Hydrate the patient before and after the examination.
- Avoid combinations with nephrotoxic medicines. If such a combination is necessary, laboratory monitoring of renal function must be intensified. The medicines concerned are in particular the aminoglycosides, organoplatinums, high doses of methotrexate, pentamidine, foscarnet and certain antiviral agents [aciclovir, ganciclovir, valaciclovir, adefovir, cidofovir, tenofovir], vancomycin, amphotericin B, immunosuppressors such as cyclosporine or tacrolimus, ifosfamide)
- Allow at least 48 hours between radiological examinations or interventions with iodinated contrast agent injections, or delay further examinations or interventions until renal function returns to baseline.
- Check for lactic acidosis in diabetics treated with metformin, by monitoring serum creatinine. Normal renal function: discontinue metformin before and for at least 48 hours after contrast agent administration or until renal function returns to baseline. Abnormal renal function: metformin is contraindicated. In emergencies, if the examination is required, precautions must be taken, i.e. discontinue metformin, hydrate the patient, monitor renal function and test for signs of lactic acidosis.
- Cardiovascular and/or pulmonary co-morbidities should be assessed before initiation of a Trans-Arterial Chemo-Embolisation procedure.
4.4.2.4. Other
Injection into certain fistulas requires the utmost caution to avoid any vascular penetration, taking into account the risk of fat embolisms.
Care should be taken not to inject the product into areas of bleeding or trauma.
4.5. Interactions with other medicinal products and other forms of interaction4.6. Pregnancy and lactation4.7. Effects on ability to drive and use machines4.8. Undesirable effects
In diagnostic radiology:
A large increase in temperature followed by a fever of 38 to 39°C may occur within 24 hours following the examination.
Fat micro-embolisms may occur, with or without symptoms. In very rare cases, they may resemble embolisms originating in the body, in terms of their appearance and size. They usually appear as punctiform opacities on radiographic images of the lungs. Transient increases in temperature are possible. Fat micro-embolisms usually occur following an overdose of contrast agent or excessively rapid infusion. Anatomic anomalies such as lymphovenous fistulas or a decrease in the capacity of lymph nodes to retain the contrast agent (in elderly patients or after radiotherapy or cytostatic therapy) favour their occurrence.
Patients with a right-to-left cardiac shunt and those with a massive pulmonary embolism are particularly at risk for fat micro-embolisms in the brain.
A temperature increase is often observed. Other more rare complications may occur, i.e. nausea, vomiting and diarrhoea.
In interventional radiology:
Most of the adverse reactions are not caused by LIPIODOL ULTRA-FLUID itself but are due to anticancer drugs or the embolisation itself.
The most frequent adverse reactions of the TACE treatment are post embolisation syndrome (fever, abdominal pain, nausea, vomiting) and transitory changes in liver function tests.
Specific adverse reactions directly related to LIPIODOL ULTRA-FLUID have not been reported.
Hyperthyroidism (see Section 4.4).
Adverse reactions are given in the following table according to system organ class and frequency, using the following classification: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1000 to < 1/100), rare (≥ 1/10 000 to < 1/1000), very rare (< 1/10 000), undetermined frequency (cannot be estimated on the basis of available data).
|
System organ class |
Frequency: adverse reactions |
|
Immune system disorders |
Undetermined frequency: hypersensitivity, anaphylactic reaction. |
|
Endocrine disorders |
Undetermined frequency: hyperthyroidism. |
|
Nervous system disorders |
Undetermined frequency: cerebral embolism. |
|
Respiratory, thoracic and mediastinal disorders |
Undetermined frequency: pulmonary embolism. |
|
Gastrointestinal disorders |
Undetermined frequency: vomiting, diarrhoea, nausea. |
|
General disorders and administration site conditions |
Undetermined frequency: fever, pain. |
|
Injury, poisoning and procedural complications |
Rare: spinal cord injury. Undetermined frequency: fat embolism. |
Adverse reactions in children
The types of adverse reactions to LIPIODOL ULTRA-FLUID are the same as those reported in adults. Their frequency cannot be estimated on the basis of available data
Write a review
Your Name:Your Review: Note: HTML is not translated!
Rating: Bad Good
Enter the code in the box below: